Definition of Infertility
There is no standard definition for Infertility. But most often, if you are under 35 years of age and have not conceived after a regular and contraceptive free intercourse for a year, you are generally considered eligible for treatment by an Infertility Specialist. Over the age of 35, the waiting period is usually six months.
Before you read any further, you should know that Fertility problems are nobody’s fault. It is a medical condition affecting almost one in six couples so you are not alone.
There are many good reads about Infertility and it’s causes across the web so we assume that you have read most of those. Our idea here is to present the data in a format that is easy to understand. We do not to wish overwhelm you with medical terminologies and concepts, sometimes ignorance is a bliss.
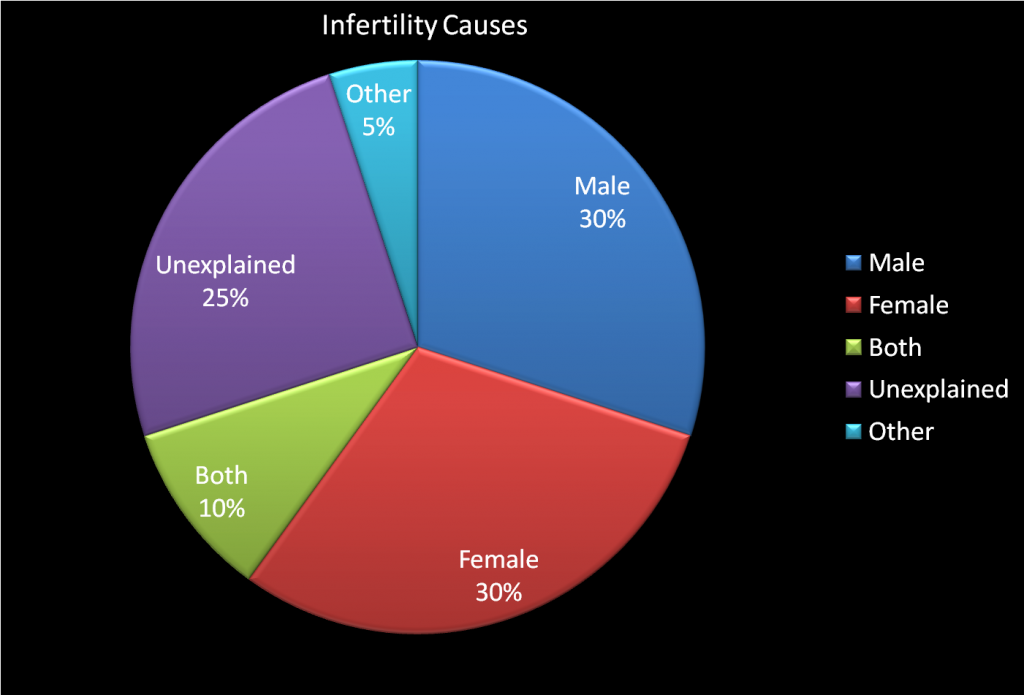
Following chart shows the gender bifurcation of the infertility causes. Men and Women equally contribute to the Infertility Causes and for a larger percentage of time the clinical diagnosis of Infertility cannot be made and hence the reasons are termed as ‘Unexplained‘. We know it is frustrating but not everything can be explained.
Female Infertility Causes
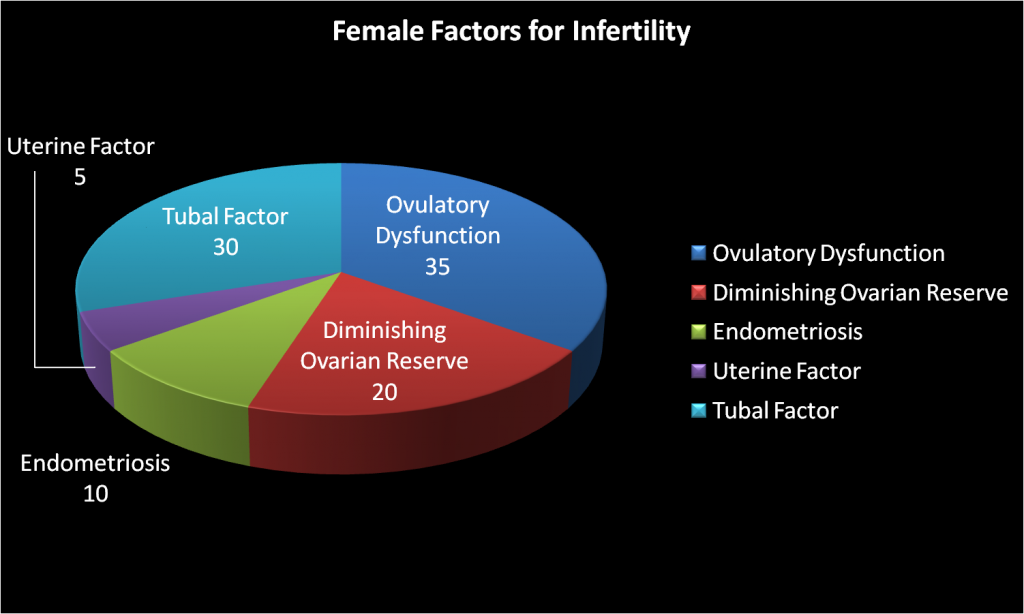
If we drill down the Infertility causes by gender, then the following chart shows the common causes that slows down conception in women:
Types of Ovulatory Dysfunction
POLYCYSTIC OVARIAN SYNDROME (PCOS)
Defined as a combination of menstrual problems (Scanty, infrequent, delayed or at times absence of periods), weight gain, infertility and a rise in the male hormone levels in the body. Also associated with an ultrasound image of ovary with excessive number of small follicles
Statistics related to PCOS
Common disorder affecting about 20 % of the females visiting a fertility clinic. Incidence on the rise due to lifestyle changes and obesity.
Common Symptoms of PCOS
- Menstrual Irregularity: Scanty, infrequent, delayed or at times absence of menses.
- Obesity
- Infertility
- Excessive hair growth
Causes of PCOS
Thought to be both inherited as well as affected by lifestyle.
Diagnosis of PCOS
Clinical and by Ultrasound. Hormone tests rarely required.
Treatment of PCOS
- Lifestyle changes (Exercise and Weight Loss)
- Induction of Ovulation, Follicular Monitoring, IUI
- If ovulation does not occur with oral medicines, injections (Gonadotropins) may be required. In severe cases which do not respond to medicines, Laparoscopic Surgery is recommended.
- If Ovarian Hyperstimulation occurs, IUI can be converted into IVF
Likelihood of Pregnancy Post Treatment of PCOS
Very Good. Ovarian Stimulation more effective if life style changes are incorporated concurrently.
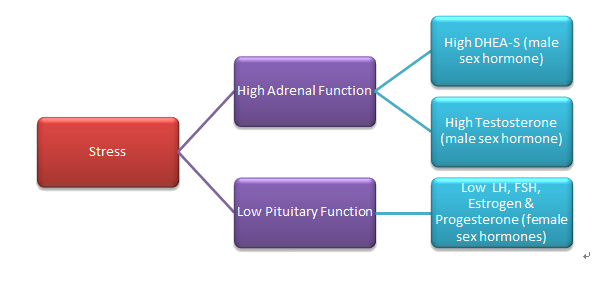
Stress directly affects your body and your Fertility. Here’s how!
ENDOMETRIOSIS
When the cells from the uterine lining start growing outside the uterus, for example in the peritoneum, fallopian tubes, ovaries, bladder or intestines
Statistics on Endometriosis
10% of Normal Female Population and up to 20% of Females with Infertility face this problem
Common Symptoms for Endometriosis
- Recurring Pelvic Pain
- Mild to severe cramping on both sides of Pelvis
- Extremely painful cramping during menses (dysmenorrhea)
- Painful intercourse (dyspareunia )
- Urgency in urination, frequent urination (dysuria)
Causes of Endometriosis
- Genetic Predisposition
- Environmental Toxins like Dioxins
- Aging
Diagnosis of Endometriosis
Symptoms of Endometriosis
Laparoscopy is considered the Gold standard for diagnosing endometriosis
Treatment for Endometriosis
Laparoscopic treatment (cauterization) of endometriotic spots
Ovarian Stimulation and Intrauterine Insemination (IUI) : Cost Effective and appropriate first line of treatment as it increases the chances of pregnancy per cycle
IVF may required in severe cases where endometriotic adhesions are dense.
Likelihood of Pregnancy Post Treatment
Very Good Pregnancy rates after treatment.
Early treatment and conception recommended as the disease is progressive in nature. Pregnancy itself is a good cure for the disease and therefore most of the symptoms like painful periods, pelvic pain etc are relieved after pregnancy.

DIMINISHING OVARIAN RESERVE OR LOW AMH
What is Primary Ovarian Insufficieny or POI
When the number of eggs in the ovary are reduced. In most cases leads to premature loss of ovarian function (premature ovarian failure at less than 40 years of age).
Statistics related to Ovarian Failure or POI
Accounts for 20% of all cases of female infertility.
With an increase in age the number of eggs decreases. The rate of fall accelerates after the age of 32-33 leading to sterility at a mean age of 41.
Common Symptoms of low ovarian reserve
Only extreme degree of diminished ovarian reserve is symptomatic. This stage is characterized be peri-menopausal symptoms like hot flushes, night sweats, mood swings, painful intercourse due to vaginal dryness, exhaustion and similar symptoms
Causes of low ovarian reserve
- Genetic/Familial: Daughters have menopause earlier if mothers have had early menopause
- Autoimmune: Some autoimmune diseases are linked with loss of ovarian function
- Chemo or Radiotherapy induced: Used as a part of anti-cancer treatment
Diagnosis of POI or Ovarian Failure
- Menstrual History: Irregular cycles
- Ultra Sound: Small ovaries, Reduced antral follicle count
- Hormones: Raised FSH, LH. Low AMH and Estradiol
Treatment of low ovarian reserve
Attain pregnancy as soon as possible, may require ovarian stimulation with IUI to increase chances of conception per cycle. Supplementation with DHEA therapy is recommended for expected poor responders
Likelihood of Pregnancy Post Treatment for low AMH
Very good till treatment is carried out in a timely manner. Once ovarian reserve is depleted, IVF with oocyte donation gives good results.
POOR EGG QUALITY
Microscopic evaluation of egg showing abnormal appearance indicating low fertilization ability
How common is poor quality of oocyte or eggs ?
Increasing as age of attainment of pregnancy is on the rise. No exact figures available.
Common Symptoms related to poor quality of eggs
Infertility
Repeated implantation failures
Premature menopause
Causes of poor quality of eggs
Age: Commonest cause of deterioration of quality of egg.
Local pathology like Endometriosis, Pelvic Inflammatory Disease (PID), Genital Tuberculosis
Systemic Disorders: Autoimmune Disorders, Endocrinological abnormalities like High Prolactin levels
Diagnosis of poor quality of oocytes or eggs
Menstrual History: Irregular cycles
Ultra Sound: Small ovaries, Reduced antral follicle count, unruptured follicles noted during follicular monitoring
Hormones: Raised FSH, LH. Low AMH and Estradiol, High Prolactin
During IVF after oocyte retrieval, when the eggs are viewed under magnification
Treatment for poor quality of eggs
Supplement with Anti oxidants, DHEA. Correct reversible causes like like High Prolactin levels. If uncorrectable cause or If oocyte quality remains poor inspite of treatment, oocyte donation with IVF
Likelihood of Pregnancy Post Treatment
Very Good either with own eggs or if own eggs have lost fertilization ability, with donor eggs and IVF
OVULATION ABNORMALITIES
Any disorder in the process of release of egg form the ovary.
Can range from irregular ovulation (Oligo-ovulation) to complete absence of ovulation (An-ovulation)
Statistics related to Ovulation Abnormalities
Accounts for 35% of causes of infertility amongst women
Common Symptoms of Ovulation Abnormalities
Delayed or absent menstrual cycles
Causes of Ovulation disturbances
Hormonal Derangements (Thyroid, Prolactin)
Age: increased ovulation abnormalities as age increases
Diagnosis of Ovulation disturbances
Menstrual History: Irregular, Infrequent or absent menses
Serum Progesterone : At least one week before expected day of menses, less than 3ng/ml best hormonal marker for anovulation
Ovulation prediction kits or LH kits: Failure of positive test
Endometrial Biopsy: Rarely done nowadays for ovulation prediction as it is an invasive procedure. When done, absence of secretory changes in endometrium indicate anovulation
Ultrasonography: Best indicator nowadays. Indicates absence of any growing follicle when monitored from day 9 of menses onwards.
Treatment of ovulation disturbances
Induction of ovulation with medicines or injections after correction of pre-existing abnormality if any.
Likelihood of Pregnancy Post Treatment of Ovulation dysfunction
Very good if induction of ovulation sucesssful

FALLOPIAN TUBE BLOCKAGE
Blockage of the Fallopian Tube or severe damage to the inner lining of the Fallopian tube making it nonfunctional.
Statistics related to Tubal Blockage
Accounts for 30 % of all cases of female infertility.
Common Symptoms of Fallopian Tube Blockage
Rarely symptomatic. Mostly presents as inability to conceive. In some cases can cause lower abdominal pain if associated with pelvic inflammatory disease (PID)
Causes of Fallopian Tube Blockage
Infections: Genital Tuberculosis, Chlamydia, Sexually Transmitted Diseases
Structural: Surgical procedures, endometriosis, tubal ligation etc.
Diagnosis of Tubal Blockage
Endometrial Biopsy for detection of Tuberculosis, Hystero Salpingo Graphy (HSG), Sono Salpingo Graphy (SSG), Laparoscopy (Gold Standard)
Treatment for Blocked Tubes
Laparoscopic release of adhesions, restoring normal tube-ovary relationship, Opening of fimbrial ends of the fallopian tube and similar endoscopic procedures. In some cases, laparoscopic correction may not be possible due to extent of damage to the tubes. In all such cases, IVF is the treatment of choice.
Likelihood of Pregnancy Post Treatment of Tubal Blockage
If minor adhesions are corrected surgically, chances of spontaneous conception are very good. If significant loss of tubal function exists, Good Pregnancy rates with IVF.
Male Infertility
In approximately 40 percent of infertile couples, the male partner is the sole cause and in 20 percent a contributing cause, of infertility. Despite the male factor being at least partly responsible in about 60 percent of infertile couples, infertility evaluations have traditionally focused on women, because women tend to seek Gynaecological care and because men often are reluctant to seek advice.
A variety of disorders ranging from hormonal disturbances to physical problems, to psychological problems can cause male infertility. Although many treatment options are now available, in many cases treatment will not work.
In many instances, male infertility is caused by testicular damage resulting in an inability of the testicle to produce sperm. Once damaged, the testicle will not usually regain its sperm-making capabilities; this aspect of male infertility is analogous to menopause (though not natural like menopause) for women and cannot usually be treated.
Despite medicine’s limited ability to treat male infertility, many successful treatment options are available today for its many causes. Besides testicular damage, the main causes of male infertility are low sperm production and poor sperm quality.
Causes of Male Infertility
Male factor infertility refers to the failure of a couple to achieve conception due to problems specifically related to the man’s sperm, seminal fluid, or reproductive organs. A number of things can affect sperm count, ability to move (motility) or ability to fertilize the egg. The most common causes of male infertility include:
1. Abnormal sperm production or function due to various problems, such as undescended or torsion testicles, varicocoele, genetic defects such as Klinefelter’s Syndrome, hormonal disorders (which may also disturb libido and cause impotence) such as hyperprolactinemia, hypothyroidism, congenital adrenal hyperplasia, hypogonadotropic hypopituitarism and panhypopituitarism or infections such as mumps, tuberculosis, brucellosis, gonorrhea, typhoid, influenza, smallpox, and syphilis.
2. Problems with the delivery of sperm due to sexual problems, such as erectile disfunction, premature ejaculation, ejaculatory incompetence or painful intercourse (dyspareunia); health issues, such as retrograde ejaculation; certain genetic diseases, such as cystic fibrosis; or structural problems, such as blockage of the part of the testicle that contains sperm (epididymis). Scarring from tuberculosis or some STDs like gonorrhea and chlamydia may block the epididymis or tubes.
3. General health and lifestyle issues, such as poor nutrition, obesity, stress, or use of alcohol, tobacco and drugs.
Overexposure to certain environmental hazards and toxins, such as pesticides, lead, paint, radiation, radioactive substances, mercury, benzene, boron, and heavy metals.
Ageing Male. Men older than age 40 may be less fertile than younger men.
Test's for Evaluating Male Infertility
Because the end results of the many disparate problems that cause male infertility are low sperm count, abnormal sperm shape, and poor sperm motility, additional tests besides a semen analysis are required to pinpoint the cause of the infertility. For a man to be fertile, the testicles must produce enough healthy sperm, and the sperm must be ejaculated effectively into the woman’s vagina. Tests for male infertility attempt to determine whether any of these processes are impaired.
- General physical examination. This includes examination of your genitals and questions concerning your medical history, illnesses and disabilities, medications, and sexual habits.
1. Semen analysis. This is a very important test for the male partner. Your doctor may ask for one or more semen specimens. Semen is generally obtained by masturbating or by interrupting intercourse and ejaculating your semen into a clean container. A laboratory analyzes your semen specimen for quantity, colour, and presence of infections or blood. Additional specialized sperm functional tests such as post-coital/cervical mucus test or sperm penetration assay may be done, if semen analysis is normal.
2. Hormone testing. A blood test to determine the level of testosterone and other male hormones is common.
3. Doppler evaluation of the testis and Transrectal Ultrasound. Doppler/Ultrasound can help your doctor look for evidence of conditions such as retrograde ejaculation and ejaculatory duct obstruction.
Treatment of infertility involves comprehensive evaluation of both male and female to find an ideal solution to the couple’s problem.
General Sexual Problems
Addressing impotence or premature ejaculation can improve fertility. Treatment for these problems often is primarily with medication or behavioural approaches, though mechanical and surgical treatment is sometimes effective. Artificial insemination with an ejaculate (like in Intra Uterine Insemination-IUI ) can be used to overcome infertility.
Treatment of Male Infertility
Treatment of male infertility depends on the cause, how long you’ve been infertile, your age and your partner’s age, and many personal preferences. Some causes of male infertility can’t be corrected. However, a woman can still become pregnant with assisted reproductive technology or other procedures to restore fertility.
Simple lifestyle changes, like abstaining from alcohol, tobacco, and illicit drugs can improve male fertility. A healthy diet, sufficient (not excessive) exercise, and proper amounts of vitamin B12, vitamin C, and zinc also improve fertility.
Treatment for Low Sperm Count or oligozoospermia
- Hormonal treatment if needed – usually in 5% of men
- Surgical treatment of varicocele
- Ejaculatory duct incisions
- Medical treatment
- Sperm concentration methods
- Electro Ejaculation
Cases of known Cryptozoospermia and Necrozoospermia are also treated with medicine and/or surgical intervention.
Treatment for No Sperm Count or Azoospermia
- If due to blockage – Microsurgical Bypass operations
- Micro Epididymal Sperm Aspiration (MESA)
- Bilateral testicular biopsies (TESA)
Donor Insemination - When is it recommended?
Therapeutic donor insemination (TDI) or Donor Sperm can be considered for many causes of male infertility as mentioned below:
- Irreversible Azoospermia
- Severe Oligozoospermia
- Poor motility and abnormal morphology of sperm
- Known genetic disorders in the male e.g. Huntington’s disease, hemophilia etc.
- Males with non-correctable ejaculatory dysfunction (ED) secondary to trauma, surgery or drugs, neurological disease, spinal chord injuries, etc.
- Reproductive option after radiation or chemotherapy
- Severely Rh-sensitized Rh-Negative women with an Rh-Positive partner
