
Semen Analysis may seem like a pretty simple test for assessment of male fertility, but Semen Analysis test, if not done by an experienced lab technician and at an Andrology Lab that lacks basic understanding of male gametogenesis, the results may impact your fertility treatment and eventually the success of your IVF treatment. Here’s how.
Significance of maintaining proper abstinence
A shorter abstinence may impact the volume of sample and the concentration of sperm in the sample, but it enhances the motility of the sperm. Hence if your previous reports have reported lower motility, try maintaining a shorter abstinence.
The recommended abstinence period for a Semen Analysis test is 2 to 5 days, however, make sure that you maintain similar abstinence for repeat testing.
Significance of Volume during Semen Analysis
Very low semen volume could be a result of improper collection of semen sample, please report such an incidence to the lab technician.
Low volume assessed during Semen Analysis may also indicate obstruction of ejaculatory duct or poorly developed Vas Deferens. At times low semen volume may also indicate partial retrograde ejaculation.
Very high semen volume may indicate active inflammation of accessory organs. Hence volume of semen should be correlated with other parameters to rule our any infection in reproductive organs.

Advanced Semen Analysis
Advanced Reporting - WHO 6th Edition
Same Day Online Reporting
Book My AppointmentRuling out infection during Semen Analysis
Advanced Semen Analysis measures the sperm concentration, motility and morphology as well as vitality as per the World Health Organization (WHO Manual version 6 released in 2021).
Presence of infection in the semen sample is indicated by investigating the colour of the sample, abnormal pH, volume of the sample as well as presence of leukocytes in the sample.
It takes an experienced technician to co-relate the pH, appearance as well as count of round cells in the sample and reach to an inference that the sample needs to be tested for leukocytes.
Reports that show abnormally high count of leukocytes and/or abnormal pH indicate presence of infection in the semen sample. This condition is usually treated by antibiotics by the doctor.
Abnormally high leukocytes are also responsible for generation of high ROS which eventually damages sperm DNA.
Importance of noting liquefaction
Inadequate liquefaction in presence of coagulum, may indicate deficiency of prostatic enzymes. At the same time watery semen may indicate absence or obstruction in the seminal and/or ejaculatory ducts.
Ruling out agglutination due to Sperm Antibodies
Agglutination is defined as sperm clumping to other sperm, head to head, head to tail, or tail to tail, may indicate the presence of sperm antibodies in the semen.
There is a difference between aggregations and agglutinations, aggregations are when dead sperm sticks to debris in the semen sample.
Hence an experienced technician can differentiate between the two and report the correct type of agglutination.
Presence of anti-sperm antibody can affect the motility of the sperm and it’s interaction with the oocyte. Presence of agglutination is rare, but needs to be reported appropriately, because the choice of treatment depends on that.
Proper assessment of Motility as per WHO manual 6th Edition
Not all labs measure motility as per WHO Manual 6th edition. This results in the forward motility being assessed as one percentage, instead of sub-dividing the progressive motility into rapid-progressive and slow-progressive.
Rapid progressive sperms are capable of negotiating the cervical mucus and reach the site of fertilization in time. Hence measurement of rapid progressive sperms is clinically important as it helps in deciding the treatment choices in terms of timed intercourse, IUI or IVF / ICSI.
Proper Assessment of Sperm Morphology
One major change in WHO Manual 6th Edition has been removal of the Kruger’s Strict Morphology assessment and replacing it with assessment of typical forms. Typical forms are defined as shape of normal spermatozoa found in fertile men.
Another change in the WHO 6th Edition assessment during the morphological assessment is noting the Extra Residual Cytoplasm of the Sperm Head as it is believed to contribute to the generation of excessive ROS in semen, which in turn damages the sperm DNA. Make sure these parameters are tested and reported.
Assessment of samples with No or Nil Sperm
When it comes to Azoospermia (Nil Sperm or No Sperm seen in Semen Sample), the confirmation of the diagnosis needs very precise assessment of the complete semen sample. There should be no scope of error in reporting because the patient’s fatherhood is at stake.
If no sperm has been seen on one slide of the sample, make two more slides for proper assessment. If no sperms are seen in all three slides / wet preparation, then proceed to centrifuge the sample and assess every drop of the pellet patiently.
Another major mistake that we often see in reports from many labs is not testing fructose for samples where no sperms are seen. Testing for presence or absence of Fructose is absolutely essential for any semen sample that has absence of sperms.
If the sample volume produced is too less, it may indicate a case of retrograde ejaculation and proper test needs to be done to confirm the same.
Proper reporting of samples like Azoospermia or Cryptozoospermia is of paramount importance because the treatment choice and success of the IVF-ICSI or TESA treatment is dependent on these lab results.
Assessment of samples with low motility
Semen samples showing low forward motility, i.e. motility less than 40% should be tested for Vitality or Viability. This test is performed to differentiate between immotile-dead and immotile-live sperms.
Presence of large proportion of immotile but live sperm is indicative of structural defect in the flagellum (tail) of the sperm. However presence of large proportion of immotile and dead sperm may be indicative of epididymal pathology or an immunological reaction to an infection.
Experience to report rare Sperm Abnormalities to Clinician
Cases like Globozoospermia (Round headed spermatozoa lacking acrosome) are very rare. This condition affects less than 0.1% Men in Infertile group. You need a very trained Andrology lab technician to detect such an abnormality and report it. Lack of acrosome means that fertilization of oocyte will not be possible by IUI or IVF and it will need special way of doing ICSI.
Complete Asthenozoospermia Vs Necrozoospermia
Both these conditions are very rare and affects less than 1 in 5000 men. Both these conditions present a semen sample with 100% immotile sperms. However, vitality testing result differentiates between the two cases.
Samples with 100% immotile and dead sperms are labelled as Necrozoospermia. While samples that show completely immotile sperms but have some live sperms are categorized as Complete Asthenozoospermia.
The treatment choices for Complete Asthenozoospermia is different from Necrozoospermia, hence proper reporting is absolutely essential for both.
Sperm DNA Fragmentation Index (DFI) testing
Unfortunately, no physical parameter in the semen sample or sperm morphology indicates higher DFI, but repeated miscarriage should be an indicator for high sperm DFI and hence DFI may be tested.
DFI test results show high inter-operator variability and hence should be preferably done from labs with experienced andrology lab technicians.
Do you need other sperm function tests?
There are many sperm function tests that can be performed to understand the sperm function better, few of them are listed below:
- HOS Test or Viability Testing
- ROS Assessment
- Test for Sperm Capacitation
- Sperm Penetration Assays
- Sperm FISH
Whether such tests are needed or not is debatable. A routine semen analysis, if done well, tells a lot about your fertility potential, hence choose a lab where the test results are discussed with the Clinician / Doctor by the lab technician before the report has been released.
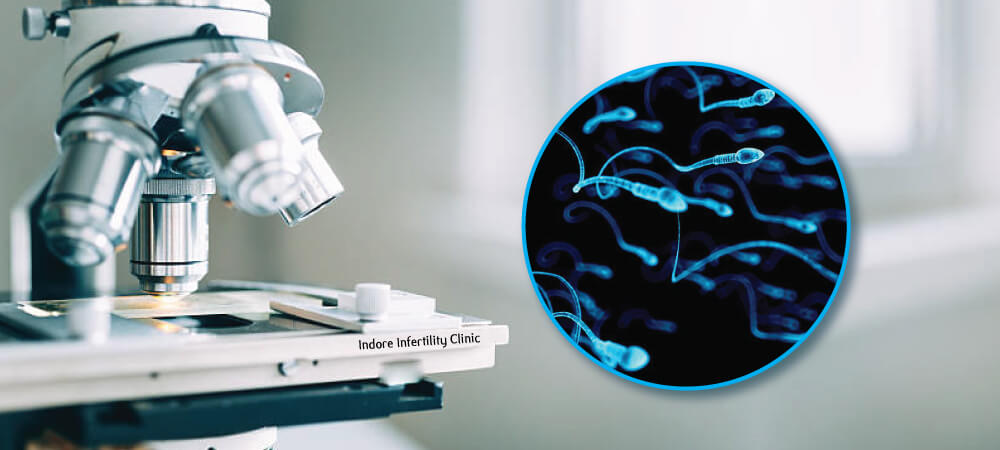
What is the typical cost of Semen Analysis Test in Indore?
Routine Semen Analysis ranges from INR 200 to INR 500. However, since the course of your IVF ICSI treatment depends on the results of this test, it is best to get the Semen Analysis done from an Andrology lab associated with an Infertility Centre. They usually have better microscopes and experienced Embryologist’s who are trained to deal with sperms, and they understand the significance of reporting not only the motility and concentration of the sperm, but the importance of liquefaction, agglutination, round cells etc. in the sample.
And since the andrology lab technicians are in direct touch with the clinician, they can always have a direct word with the Clinician to communicate each report in person. There is a difference between routine semen analysis and Advanced Semen Analysis, and hence Advanced Semen Analysis cost’s a bit more than routine.
We at Indore Infertility Clinic, follow guidelines of WHO Manual 6th Edition for reporting findings of Semen Analysis and each report is discussed and communicated to the Fertility Specialist before releasing the report. We charge INR800 for our Advanced Semen Analysis Test.
Final Words of Advice
Infertility treatment is not just about being fixated to one partner’s gamete, it is about taking a holistic approach to the situation and offering treatment choices based on multiple factors that also include time to get successful result as well as financial burden on patients. Hence discuss your options very honestly with the doctor and trust that the doctor has your best interest in his mind.
WHATSAPP FOR MORE INFORMATION