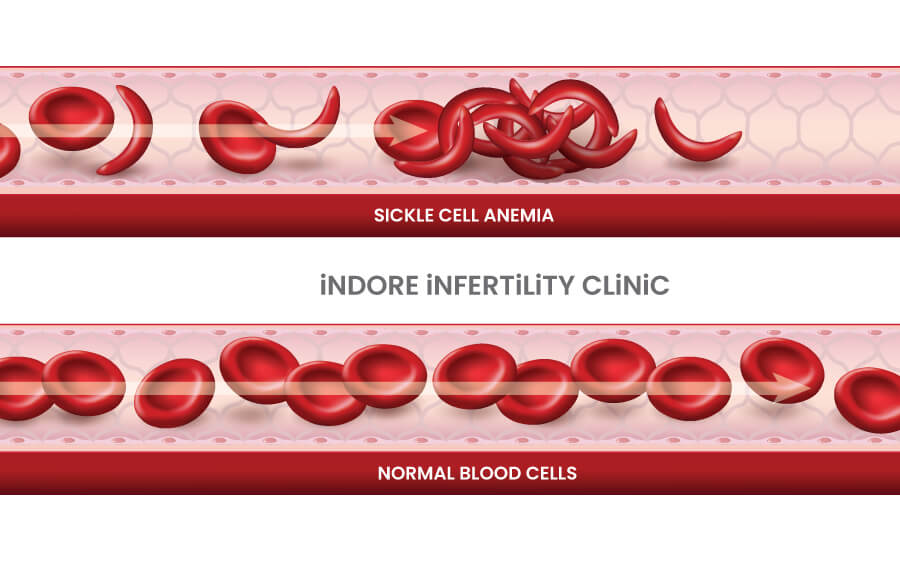
Sickle-cell anaemia is a genetic blood disorder that affects the haemoglobin which is a protein in red blood cells responsible for carrying oxygen throughout the body. In individuals with sickle cell anaemia, a specific mutation in the haemoglobin gene causes the red blood cells to take on a crescent or sickle shape instead of their normal round shape. This abnormal shape hinders the cell’s flexibility, leading to various complications.
Sickle-cell anaemia is caused by an inherited genetic mutation, meaning it is passed down from parents to their children. If both parents carry the sickle cell trait, there is a 25% chance with each pregnancy that their child will have sickle cell anaemia. To know more about genetic diseases please read our blog about the same.
What problem does sickle cell anemia cause in our body ?
- Pain Crises: The misshapen red blood cells can get stuck in blood vessels, causing sudden and severe pain known as pain crises.
- Anaemia: The abnormal cells break down more quickly than normal cells, leading to a shortage of red blood cells and anaemia, resulting in fatigue and weakness.
- Organ Damage: Sickle cells can block blood flow, leading to damage in various organs, including the lungs, heart, kidneys and spleen.
- Infections: Individuals with sickle cell anaemia are more susceptible to infections due to a compromised immune system.
Understanding the causes and effects of sickle cell anaemia is crucial for individuals and families affected by this condition. Seeking guidance from healthcare professionals, including genetic counsellors, fertility specialists and haematologists, is essential for managing the complications associated with sickle cell anaemia.
How common is Sickle-Cell Anemia?
Sickle cell anaemia is a relatively common genetic disorder, particularly in regions where malaria is or was prevalent. Here are the figures to provide a perspective:
Worldwide:
- Globally, it is estimated that over 300,000 babies are born with sickle cell anaemia each year.
- Approximately 5% of the world’s population carries a gene for haemoglobin S, the genetic mutation responsible for sickle cell disease.
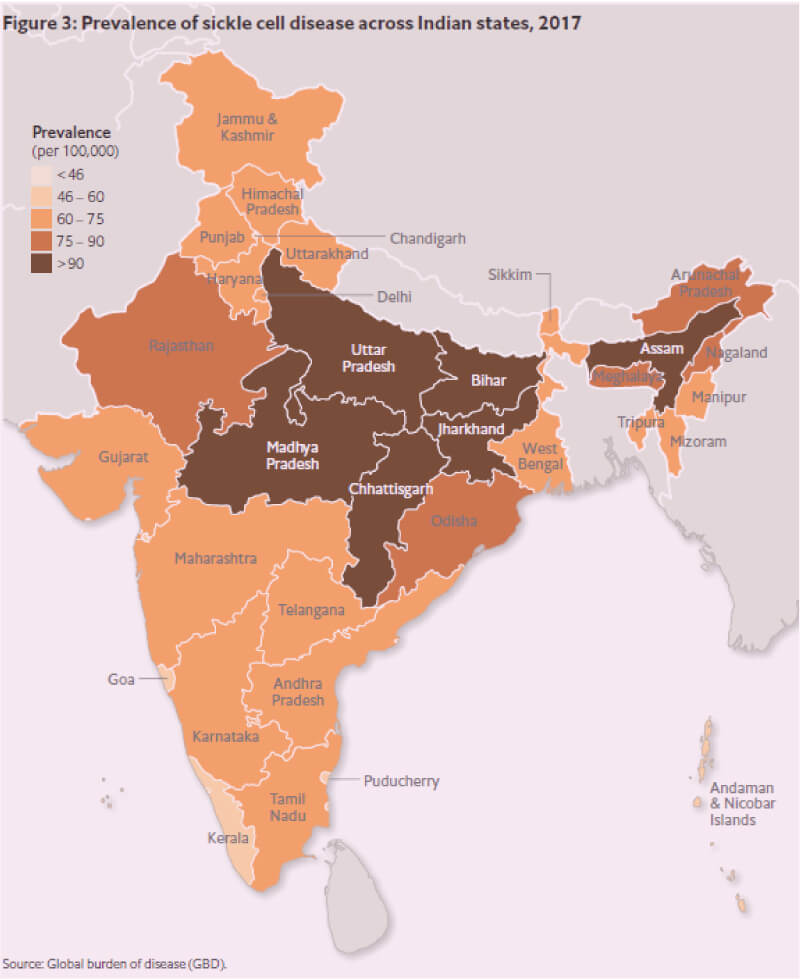
In India:
- In India, the prevalence of sickle cell anaemia varies across different regions. It is more commonly found in tribal communities.
- The overall carrier rate of the sickle cell trait in India has been reported to range from 1% to 40% in various populations.
These figures emphasize the significant impact of sickle cell anemia the need for awareness, genetic testing and appropriate healthcare interventions, particularly in regions with a higher prevalence of the disease.
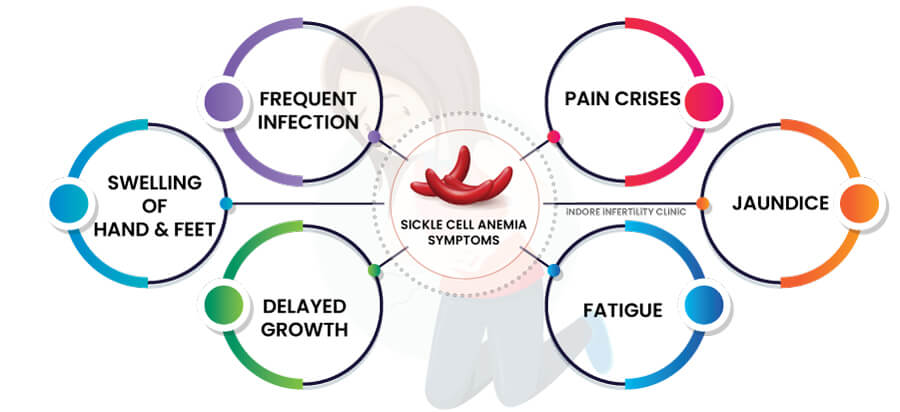
What are the symptoms of Sickle-Cell Anaemia?
Sickle cell anaemia presents with various symptoms, and the severity can vary among individuals. Here is an overview of the common symptoms:
- Pain Crises: Sudden and severe episodes of pain, known as pain crises, are a hallmark of sickle cell anaemia. These crises can affect bones, joints, and the abdomen.
- Fatigue: Anaemia, caused by a shortage of red blood cells, leads to fatigue and weakness.
- Jaundice: Sickle cell anaemia can cause the breakdown of red blood cells, leading to jaundice, characterized by yellowing of the skin and eyes.
- Swelling of Hands and Feet: Swelling, particularly in the hands and feet, can occur due to reduced blood flow caused by sickle-shaped cells.
- Frequent Infections: Sickle cell anaemia can compromise the immune system, leading to an increased susceptibility to infections.
- Delayed Growth: In children, sickle cell anaemia can impact growth and development.
Recognizing these symptoms is crucial for early intervention and effective management of sickle cell anaemia. Individuals experiencing these symptoms, especially those with a known family history of the condition, should seek medical attention for proper diagnosis and care.
What Do You Need to Know About the Genetic Basis of Sickle-Cell Anamia ?
Genetic Mutation: A genetic mutation refers to a change in the DNA sequence, which can affect the structure and function of a gene.
In sickle cell anaemia, there is a specific mutation in the haemoglobin gene that leads to the production of abnormal haemoglobin called haemoglobin S.
Inheritance Pattern – Autosomal Recessive: Autosomal recessive inheritance means that two copies of a mutated gene (one from each parent) are needed for the disorder to manifest.
In sickle cell anaemia both parents must carry a copy of the mutated gene. If both parents are carriers, there’s a 25% chance with each pregnancy that the child will inherit two copies of the mutated gene, leading to sickle cell anaemia.
Carrier and Sickle Cell Trait: A carrier is an individual who has one normal gene and one mutated gene for a particular trait but does not display symptoms of the disorder. Carriers of the sickle cell trait usually do not have the disease but can pass the mutation to their children.
Understanding these terms provides insight into the genetic basis of sickle cell anaemia and empowers individuals to make informed decisions about family planning and healthcare.
Is Sickle Cell Anaemia the Same as Sickle Cell Disease?
Yes, “sickle cell anaemia” and “sickle cell disease” are terms often used interchangeably, but there is a subtle difference in their meanings.
Sickle Cell Anaemia: Sickle cell anaemia refers specifically to one form of sickle cell disease.
It is a type of sickle cell disease characterized by the presence of two copies of the haemoglobin S mutation (HbSS) in an individual’s genetic makeup.
Sickle Cell Disease: Sickle cell disease is a broader term.
It includes various forms of the disorder, each associated with different combinations of haemoglobin mutations. In addition to sickle cell anaemia (HbSS), there are other forms like HbSC, HbSβ-thalassemia, and more.
Thus, all individuals with sickle cell anaemia have sickle cell disease, but not everyone with sickle cell disease has the specific form known as sickle cell anaemia. The distinction lies in the specific combination of haemoglobin mutations an individual inherits. Both terms, however, are commonly used to describe the overall group of genetic disorders characterized by abnormal haemoglobin and sickle-shaped red blood cells.
What Are the Causes of Sickle Cell Anemia?
Sickle cell anaemia is caused by a specific genetic mutation that affects the production of haemoglobin; the protein responsible for carrying oxygen in red blood cells. Here’s a simplified explanation of the causes.
Haemoglobin S and Red Blood Cells: Haemoglobin S, the abnormal haemoglobin produced due to the mutation, causes red blood cells to take on a sickle shape under certain conditions. This sickle shape reduces the flexibility of the red blood cells, leading to various complications such as pain crises, anaemia, and organ damage.
sickle cell anaemia is primarily caused by the inheritance of two copies of the mutated gene from both parents, and this is crucial for individuals and families to understand, as it guides genetic counselling and family planning decisions. Genetic testing helps identify carriers and assess the risk of having a child with sickle cell anaemia.
How can you find out if you have SCD or sickle cell trait?
Determining whether you have sickle cell disease (SCD) or carry the sickle cell trait involves various diagnostic tests. Following can be used to find out if you have Sickle cell disease:
Medical Evaluation: If you experience symptoms associated with sickle cell disease or if there’s a concern based on family history, your doctor may order specific tests.
- Blood tests, including haemoglobin electrophoresis (Hb Electrophoresis), can help identify the type of haemoglobin present in your blood.
Genetic Testing: Genetic testing involves analysing your DNA to identify specific mutations associated with SCD or the sickle cell trait.
- Process: A blood sample is typically collected for testing.
- Result Interpretation: If you have two copies of the mutated gene, you are diagnosed with sickle cell disease.
- If you have one copy of the mutated gene, you are a carrier of the sickle cell trait.
Family History: Knowing your family history can provide valuable information, especially if close relatives have been diagnosed with SCD or identified as carriers.
- A positive family history may prompt healthcare providers to recommend genetic testing.
It’s important to consult with your doctor or a haematologist, for appropriate testing and interpretation of results. Genetic counselling can also provide valuable insights, especially for individuals considering family planning or concerned about the risk of passing the condition to their children. Early diagnosis allows for better management and care for individuals with sickle cell disease.
What You Need to Know About Family Health History and Sickle-Cell Anemia?
- Knowing your family health history, especially regarding sickle cell anaemia, helps identify the risk of having the condition or being a carrier.
- Discussing family health history with relatives provides valuable information for assessing genetic risk.
- If there is no clear-cut history available, you can ask your family members if any of the directly related members had any blood disease, or needed frequent admissions for blood transfusions.
What Tests Are Available for the Diagnosis of Sickle Cell Disease?
Several tests are available for the diagnosis of sickle cell disease (SCD). Here are key diagnostic methods:
Screening tests – which indicate a high risk of having the disease
- Complete Blood Count (CBC): This standard blood test provides information about the number and types of blood cells. Individuals with SCD often have low levels of red blood cells, leading to anaemia.
- Haemoglobin Solubility Test: Similar to the Sickledex test, this measures the solubility of haemoglobin S. Positive results suggest the presence of haemoglobin S and the possibility of SCD.
- Sickle Cell Solubility Test (Sickledex): This simple and rapid test, screens for the presence of sickle haemoglobin.
Diagnostic/Confirmatory tests- tests which can tell for sure if you have sickle cell disease
- Haemoglobin Electrophoresis: This blood test separates and identifies different types of haemoglobin, including haemoglobin S (the abnormal haemoglobin in SCD).
It helps determine the types and quantities of haemoglobin present in the blood, confirming the diagnosis of SCD. Positive results indicate the likelihood of SCD, but further confirmatory tests are needed.
- Genetic Testing: Molecular genetic testing can identify specific mutations in the haemoglobin gene responsible for SCD. It confirms the presence of genetic mutations associated with SCD and can provide information about the specific type of SCD.
Newborn Screening: Many regions include SCD in routine newborn screening programs. A small blood sample is taken from the newborn’s heel, and the haemoglobin is analysed. Abnormal results may prompt further testing to confirm the diagnosis.
It’s important to note that a combination of these tests is often used for a comprehensive diagnosis. If there is a family history of SCD or if symptoms are present, your doctor may recommend specific tests to confirm the diagnosis and determine the type and severity of Sickle cell disease. Early diagnosis allows for timely intervention and management to improve outcomes for individuals with SCD.
What is the impact of sickle cell anaemia on fertility?
Sickle cell anaemia can have various impacts on fertility and reproductive health. Following are the most commonly encountered problems:
Delayed Puberty: Individuals with sickle cell anaemia may experience delayed puberty. Chronic anaemia and the overall impact of the disease on the body can affect the normal development of sexual characteristics.
Hormonal Changes: Sickle cell anaemia can disrupt normal hormonal balance. Hormonal changes may affect the menstrual cycle and ovulation in women, potentially impacting fertility.
Female Infertility: Sickle cell anaemia is not necessarily associated with infertility, but above-mentioned complications pose problems in conceiving, thus a fertility doctor should be consulted as soon as problem is faced. Factors such as chronic anaemia, organ damage, and the overall impact on health can contribute to fertility issues in both men and women.
Male Infertility: Sickle cell anaemia may affect male fertility. Chronic anaemia and impaired blood flow can contribute to erectile dysfunction, and there may be an impact on sperm production and quality.
Pregnancy Complications: Pregnancy in individuals with sickle cell anaemia can be high-risk. The disease increases the risk of complications such as preterm birth, low birth weight, and preeclampsia. Adequate prenatal care and management are crucial.
Consulting with a fertility specialist and genetic counsellor with ensure that these problems are addressed in a timely manner. If needed IVF with or without PGT can be considered.
How does sickle cell disease affect pregnancy?
Sickle cell disease (SCD) can significantly impact pregnancy, posing challenges for both the mother and the developing fetus. Following are important points to keep in mind.
- High-Risk Pregnancy: Pregnancy in individuals with SCD is considered high-risk. The underlying health issues associated with SCD, such as chronic anaemia, increased risk of infections, and potential organ damage, elevate the overall risk during pregnancy.
- Increased Risk of Pregnancy Complications: SCD increases the risk of various pregnancy complications including preterm birth, low birth weight, preeclampsia, and maternal complications such as pain crises and infections.
- Pain Crises: Pregnant individuals with SCD may experience more frequent pain crises. Pregnancy can exacerbate the risk of sickle cell pain crises.
- Anaemia: Anaemia is a common feature of SCD and may require careful management during pregnancy. Adequate monitoring and intervention are crucial to prevent complications related to maternal and fetal well-being.
- Increased Risk of Infections: Individuals with SCD have a compromised immune system, leading to an increased susceptibility to infections. During pregnancy, the risk of infections may be heightened, necessitating vigilant monitoring and preventive measures.
- Blood Transfusions: Some women with SCD may require blood transfusions.
- Increased Monitoring: Pregnancies in individuals with SCD typically involve more frequent monitoring. Regular prenatal check-ups, specialized care, and monitoring of both maternal and fetal health are crucial to address potential complications promptly.
Managing pregnancy in individuals with SCD requires a multidisciplinary approach involving obstetricians, haematologists, and other healthcare professionals. Regular prenatal care, early intervention, and a personalized care plan are essential to optimize outcomes for both the mother and the baby.
Will Someone with Sickle Cell Trait or Sickle Cell Disease Have a Baby with Sickle Cell Disease or Sickle Cell Trait?
or
Can you pass SCD or sickle cell trait to your child?
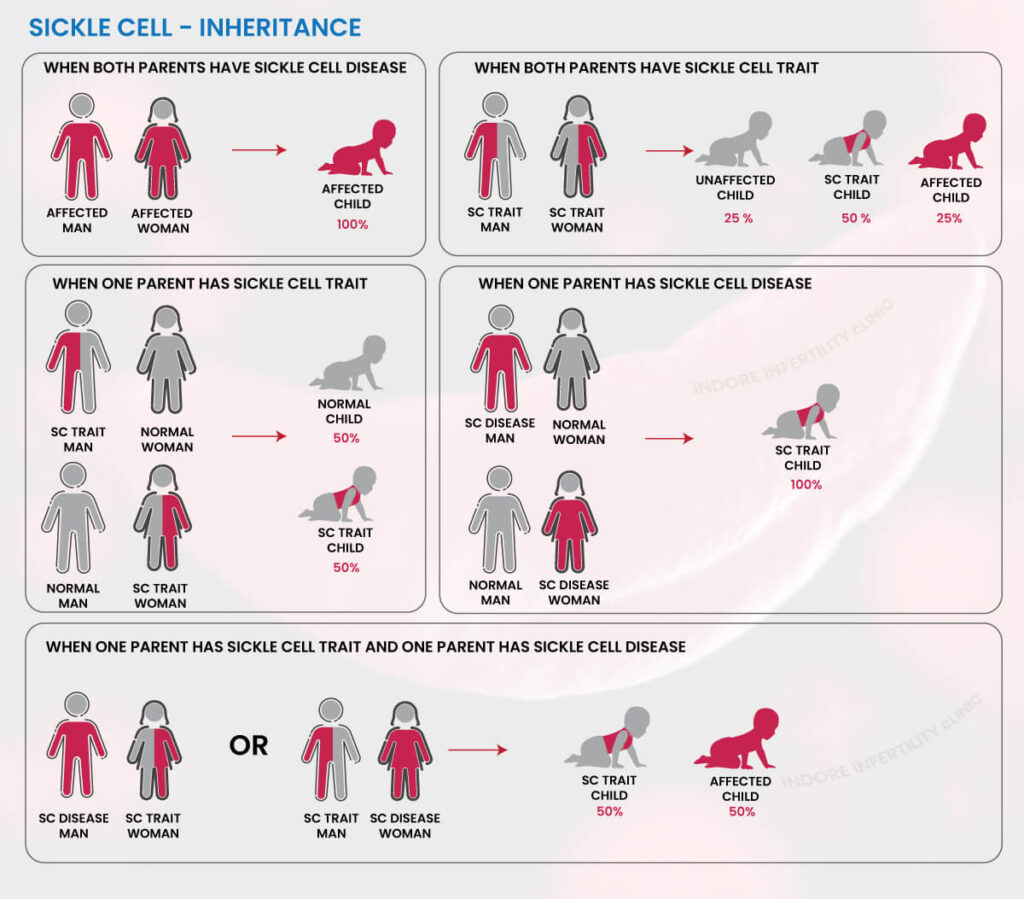
The likelihood of having a baby with sickle cell disease (SCD) or sickle cell trait (SCT) depends on the genetic status of both partners. Here are the possible scenarios:
It is important to remember that –Sickle cell disease means that the person is affected by the condition. If Sickle cell trait is found, that means that they will not have any physical symptoms, but they carry the gene with them and it can be passed on to the next generation.
Both Partners Have Sickle Cell Trait (SCT):
- There is a 25% chance of having a child with normal haemoglobin.
- There is a 50% chance of having a child with SCT.
- There is a 25% chance of having a child with SCD.
One Partner Has Sickle Cell Disease (SCD) and the Other Has Sickle Cell Trait (SCT):
- There is a 50% chance of having a child with SCT.
- There is a 50% chance of having a child with SCD.
One Partner Has Sickle Cell Trait (SCT) and the Other Does Not Carry the Trait:
- There is a 50% chance of having a child with normal haemoglobin.
- There is a 50% chance of having a child with SCT.
It’s important to understand that Sickle cell trait is a carrier status, and individuals with SCT generally do not exhibit symptoms of Sickle cell disease. However, if both partners have SCT, there is a chance of having a child with SCD.
For couples planning to have a baby and concerned about sickle cell disease, it is advisable to undergo genetic testing. Genetic testing can identify the specific haemoglobin variants present in each partner, providing valuable information about the potential outcomes for their children. Consulting with a genetic counsellor or a healthcare provider experienced in haemoglobinopathies is recommended to understand the genetic risks, explore testing options, and make informed decisions about family planning.
Can Women with Sickle Cell Trait Have a Healthy Pregnancy?
Yes, women with sickle cell trait (SCT) generally have a healthy pregnancy. Sickle cell trait is a carrier status, and individuals with SCT typically do not experience the same health challenges as those with sickle cell disease (SCD)
They should take genetic counselling before planning pregnancy. It is more important if their partner also has sickle cell trait or a related haemoglobin variant. Genetic counselling provides information about the risk of passing on certain haemoglobin variants to the baby.
Risk of Sickle Cell Disease in Offspring: If both parents have sickle cell trait, there is a 25% chance with each pregnancy of having a child with sickle cell disease.
While women with sickle cell trait generally have a lower risk of complications during pregnancy compared to those with sickle cell disease, each pregnancy is unique. It’s important for women with SCT to work closely with their healthcare providers, including infertility specialists, obstetricians and haematologists, to ensure optimal care and address any specific considerations related to their or their baby’s health.
Can Women with Sickle Cell Disease Have a Healthy Pregnancy?
Pregnancy for women with sickle cell disease (SCD) can be more complex and requires specialized care, but with proper management, many women with SCD have successful pregnancies. Here are key considerations:
- Genetic counselling and transmission risk: It is important to get counselling from genetic counsellor and discuss about the possibility of transmission of the disease, and how to avoid it. If IVF (in vitro fertilization) is being considered, PGT (prenatal genetic testing) can be concurrently used to ensure that the baby does not get the disease.
- Preconception Care: Preconception care is crucial. Women with SCD should work with their healthcare team before becoming pregnant to optimize their health.
- Medication Review: Medications may need adjustment, and vaccinations to prevent infections should be up to date.
- Regular Prenatal Care and Close Monitoring: Regular and more frequent prenatal visits are necessary to monitor the health of both the mother and the developing fetus.
- Increased Risks of Anaemia: SCD often leads to chronic anaemia, and pregnancy can further exacerbate this condition.
- Blood Tests and Blood Transfusions: Blood tests may be performed more often to monitor haemoglobin levels. In some cases, blood transfusions may be recommended to manage severe anaemia or prevent complications.
- Hydration and Nutrition: Staying well-hydrated is important to prevent sickling of red blood cells. Proper nutrition, including folic acid supplementation, is also essential.
- Pain Crises and Pain Management: Pregnant women with SCD may experience more frequent pain crises, potentially requiring hospitalization. A personalized plan for pain management should also be established with the healthcare team.
What are complications of sickle cell disease during pregnancy?
- Increased interventions, such as blood transfusions, may be necessary.
- Increased Risk of Infections: Individuals with SCD have a compromised immune system, increasing the risk of infections. Vigilant monitoring and preventive measures are essential to minimize infection risks.
- Preeclampsia: Women with SCD have an increased risk of developing preeclampsia, a condition characterized by high blood pressure and organ damage. Regular monitoring of blood pressure and early intervention may be necessary.
- Preterm Birth: Women with SCD are at a higher risk of preterm birth. Close monitoring during pregnancy and timely interventions can help manage and prevent preterm labor.
- Fetal growth restriction and Low Birth Weight: Babies born to mothers with SCD are at an increased risk of being born with low birth weight. Adequate prenatal care and monitoring can help address factors contributing to low birth weight.
- Fetal Growth Restriction: Reduced blood flow to the placenta may lead to fetal growth restriction. Regular ultrasound monitoring can help detect any issues with fetal growth.
- Increased Risk of Thrombosis: Individuals with SCD may have an increased risk of blood clot formation. Preventive measures and close monitoring for signs of thrombosis are important.
It’s important to note that while these complications may be more common in women with SCD, not every woman with SCD will experience them. Close collaboration with a healthcare team experienced in managing sickle cell disease during pregnancy, along with regular prenatal care, can help mitigate risks and improve outcomes for both the mother and the baby.
How is sickle cell disease treated in pregnancy?
The treatment of sickle cell disease (SCD) during pregnancy involves a comprehensive and individualized approach to manage the unique challenges associated with the condition. Here are key components of the treatment plan:
Preconception Care:
- Optimize the health of the woman with SCD before conception.
- Review and adjust medications.
- Ensure vaccinations are up-to-date.
- Address any chronic health issues.
Regular Prenatal Care:
- Monitor the health of the mother and the developing fetus closely throughout the pregnancy.
- More frequent prenatal visits.
- Regular blood tests to monitor haemoglobin levels.
Blood Transfusions:
- Manage severe anaemia and prevent complications.
- Blood transfusions may be advised if haemoglobin levels are critically low.
- Exchange transfusions may be used to replace sickled red blood cells with normal ones.
Hydration:
- Prevent sickling of red blood cells by maintaining adequate hydration.
- Encourage increased fluid intake.
- Intravenous hydration may be necessary during hospitalization.
Folic Acid Supplementation:
- Supports red blood cell production and prevent certain birth defects.
- Folic acid supplements are typically prescribed.
Infection Prevention:
- Minimize the risk of infections, which can be more severe in individuals with SCD.
- Ensure vaccinations are up-to-date.
- Monitor for signs of infection and treat promptly.
Close collaboration between the woman with SCD, her healthcare team, including obstetricians, haematologists, and other specialists, is essential to manage the complexities of SCD during pregnancy. The goal is to optimize maternal and fetal health while minimizing the risks associated with the condition. Individualized care plans are crucial to address the unique needs of each patient.
What Is Sickle-Cell Anaemia Genetic Testing please explain?
Sickle cell anaemia genetic testing is a diagnostic process that involves analysing an individual’s DNA to identify specific genetic variations associated with sickle cell disease (SCD). This testing aims to determine if an individual carries the genetic mutations that lead to the production of abnormal haemoglobin, causing the characteristic sickling of red blood cells in SCD.
Here’s an explanation of the key components of sickle cell anaemia genetic testing:
Genetic Counselling: To provide individuals with information about their genetic status and the potential risks associated with having children. Genetic counsellors interpret the test results, discuss the implications for family planning, and offer guidance on available options.
Genetic Analysis for Mutation: The test focuses on the genes that code for haemoglobin; the protein responsible for carrying oxygen in red blood cells. It identifies mutations in the Haemoglobin gene, which encodes the beta-globin subunit of haemoglobin. In SCD, specific mutations lead to the production of abnormal haemoglobin known as haemoglobin S (HbS).
Identification of Sickle Cell Trait (SCT) or Sickle Cell Disease (SCD): If an individual has two copies of the HbS mutation, they are diagnosed with Sickle Cell Disease (SCD). If they have one copy of the HbS mutation and one normal haemoglobin gene (HbA), they are carriers and have Sickle Cell Trait (SCT).
Sickle cell anaemia genetic testing is valuable for family planning, as it provides individuals and couples with information about their risk of having a child with SCD. Understanding one’s genetic status allows for informed decisions and, when necessary, the exploration of reproductive options that can reduce the risk of passing the condition to the next generation. Genetic counselling is a crucial component of this process, providing support and guidance for individuals and couples navigating the complexities of genetic testing and family planning.
Can you find out if your baby has SCD or sickle cell trait during pregnancy?
Yes, it is possible to find out if a baby has sickle cell disease (SCD) or sickle cell trait (SCT) during pregnancy through various prenatal testing methods.
NIPT/cffDNA testing for Sickle cell disease: It is a screening test, and it will indicate if the baby is at risk of having sickle cell disease.
- Timing: After 10 weeks of pregnancy
- Procedure: A blood sample from the mother will be taken and assessed for the sickle cell gene in the sample. If it indicates a high risk, then a confirmatory test will be advised to confirm if the baby has SCD for sure.
Chorionic Villus Sampling (CVS):
- Timing: Typically performed between 10 and 13 weeks of pregnancy.
- Procedure: CVS involves obtaining a small sample of tissue from the placenta. The tissue sample is then analysed for the presence of genetic mutations associated with SCD or SCT.
Amniocentesis:
- Timing: Usually performed between 15 and 20 weeks of pregnancy.
- Procedure: Amniocentesis involves the extraction of a small amount of amniotic fluid surrounding the baby in the womb. The amniotic fluid contains fetal cells, and genetic testing is conducted on these cells to determine the presence of genetic mutations related to SCD or SCT.
It’s important to note that both CVS and amniocentesis are invasive procedures that carry a small risk of complications. Therefore, these tests are typically offered to individuals with an increased risk of having a child with a genetic disorder, such as those with a family history of SCD or SCT, or after an NIPT indicating a high risk.
Another option for prenatal testing, especially in the context of assisted reproductive technologies like in vitro fertilization (IVF), is Preimplantation Genetic Testing (PGT).
Preimplantation Genetic Testing (PGT-M):
- Timing: Conducted before the embryo is implanted during an IVF cycle.
- Procedure: Following the fertilization of eggs and sperm in a laboratory, embryos are allowed to develop for a few days. A small number of cells are then biopsied from each embryo. biopsied cells are tested for the presence of genetic mutations, including those associated with sickle cell disease (SCD) or sickle cell trait (SCT).
- Selection of Embryos: Based on the results, only embryos without the detected genetic mutations are selected for implantation.
- Advantages: PGT offers the advantage of selecting embryos free from specific genetic disorders, reducing the risk of passing on SCD or SCT to the child.
PGT is particularly valuable for individuals or couples who are aware of their carrier status for SCD or SCT and are undergoing IVF. It allows for the identification and selection of embryos that do not carry the genetic mutations, increasing the chances of a healthy pregnancy.
Have You Explored PGT as a Solution for Sickle-Cell Anaemia?
At Indore Infertility Clinic, we understand the profound impact of genetic conditions on family planning, and we are committed to offering advanced solutions to empower your journey to parenthood. For individuals or couples who are carriers of the sickle-cell trait, we introduce Preimplantation Genetic Testing (PGT) as a powerful tool to enhance the success of your fertility treatments.
Key Benefits of PGT at Indore Infertility Clinic:
Precision Screening: PGT enables precise screening of embryos created through in vitro fertilization (IVF), identifying those without the sickle-cell anaemia mutation.
Increased Success Rates: By selecting embryos free from the genetic mutation, PGT-M enhances the likelihood of a successful pregnancy without the risk of passing on sickle-cell anaemia.
Personalized Care: Our team of experienced fertility specialists and genetic counsellors works closely with you to understand your unique circumstances and family planning goals, providing personalized guidance throughout the PGT process.
Ethical Considerations: We prioritize open and transparent discussions about ethical considerations, ensuring that you are fully informed and comfortable with every step of the process.
Your Journey, Your Decisions: We recognize that the decision to pursue PGT is deeply personal. At Indore Infertility Clinic, we are dedicated to supporting you in making informed decisions that align with your values and aspirations.
Schedule a consultation with our team to explore how PGT can be integrated into your fertility treatment plan. Our experts are here to answer your questions, address any concerns, and guide you toward a path that aligns with your dreams of a healthy and happy family.
Choose Indore Infertility Clinic for cutting-edge fertility solutions and compassionate care tailored to your unique needs. Your journey to parenthood begins with informed choices and the support of a dedicated team.
Can You Provide a Detailed Guide on Preimplantation Genetic Testing (PGT) for Sickle-Cell Anaemia?
Understanding PGT: Preimplantation Genetic Testing (PGT) is a sophisticated technique that allows for the screening of embryos created through in vitro fertilization (IVF) to identify specific genetic mutations. In the context of sickle-cell anaemia, PGT-M is advised which looks for single genes which are affected in certain diseases. PGT offers a precise and proactive approach to family planning, which can help you to protect your child from sickle cell disease.
Key Components of PGT for Sickle-Cell Anaemia:
- Genetic Counselling: Begin the PGT process with a thorough consultation with experienced genetic counsellors. Discussion Points:
- Explanation of sickle-cell anaemia and the specific genetic mutation involved.
- Understanding personal and family medical histories.
- Discussion of the implications of having a child with sickle-cell anaemia.
- IVF Process: PGT is integrated into the IVF process. Following are the steps of IVF:
- Stimulation of the ovaries and egg retrieval.
- Fertilization of eggs with sperm in the laboratory.
- Culturing embryos for a few days to allow development.
- Embryo Biopsy: Extracting a small number of cells from the growing embryo (blastocyst) for genetic testing. Procedure:
- A few cells are carefully removed from each embryo.
- The biopsied cells undergo genetic testing.
- Genetic Testing: Identify embryos without the sickle-cell anaemia mutation. Analysis of the DNA of the biopsied cells to detect the presence of the specific genetic mutation causing sickle-cell anaemia.
- Selection of Healthy Embryos: Choose embryos without the genetic mutation for implantation. Embryos identified as free from the sickle-cell anaemia mutation are selected for transfer.
- Embryo Transfer: Implant selected embryos into the uterus. One or more healthy embryos are transferred, increasing the chances of a successful pregnancy.
- Support: Ongoing support is provided throughout the pregnancy and beyond, ensuring the well-being of both the mother and the developing fetus.
What Are the Benefits and Challenges of PGT in Sickle-Cell Anemia Prevention?
Benefits of PGT in Sickle-Cell Anaemia Prevention:
Precise Genetic Screening:
- PGT allows for precise screening of embryos, identifying those without the sickle-cell anaemia mutation.
- Increased accuracy in selecting embryos that are free from the genetic mutation, reducing the risk of passing on sickle-cell anaemia.
Enhanced Success Rates:
- PGT increases the likelihood of a successful pregnancy by choosing embryos without the genetic mutation.
- Higher success rates in achieving a healthy pregnancy, minimizing the risk of having a child with sickle-cell anaemia.
Personalized Treatment Plan:
- PGT offers a personalized approach to family planning for individuals or couples who are carriers of the sickle-cell trait.
- Empowers individuals to make informed decisions aligned with their values and aspirations.
Challenges of PGT in Sickle-Cell Anaemia Prevention:
Invasive Nature of Procedures:
- Both IVF and PGT involve invasive procedures.
- Individuals may experience physical discomfort, and there is a small risk of complications associated with procedures such as egg retrieval and embryo biopsy.
Financial Considerations:
- PGT and IVF procedures can be financially demanding.
- Individuals should consider the financial aspects and explore available support, such as insurance coverage or financial assistance programs.