

Understanding Thalassemia: An Overview
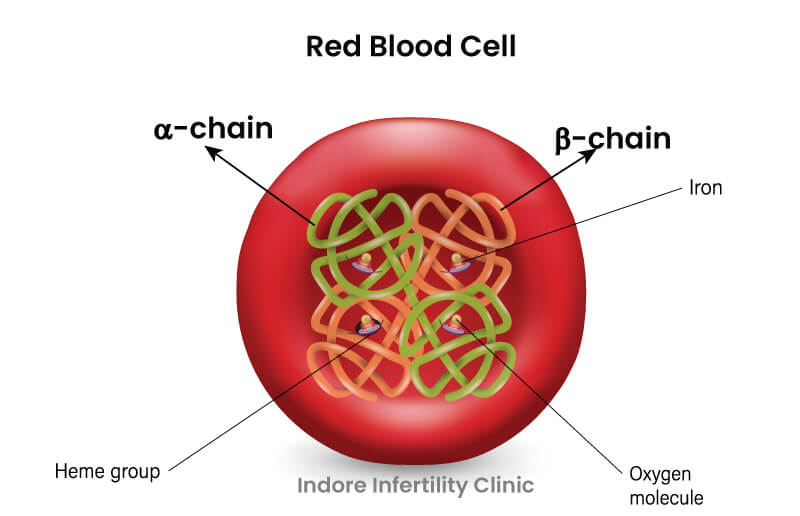
Haemoglobin is made up of some protein chains and is a delivery system for oxygen. Picture it as a four-part team, with two alpha and two beta globin (a type of protein) chains. These chains work together to grab and transport oxygen, ensuring our body gets the oxygen it needs to function properly.
Thalassemia is a genetic blood disorder that affects the production of haemoglobin. The condition arises from mutations (explained below) in the genes responsible for making haemoglobin, leading to an imbalance in the production of its components—alpha and beta globin chains. Depending on the specific gene mutations, thalassemia can result in a shortage of one or both types of these chains, disrupting the normal formation of red blood cells.
This deficiency leads to anaemia, causing symptoms like fatigue and weakness. Thalassemia has various types and severity levels. Understanding the genetic basis of thalassemia is crucial for planning treatment and management in an effected person.
In simple terms, a mutation is a change in the genetic instructions that guide the body’s functions. In the context of thalassemia, these mutations occur in the genes responsible for making haemoglobin. For further understanding of genetic diseases please read our previous blog on the topic.
How common is Thalassemia ?
Thalassemia is a globally widespread genetic disorder, with an estimated 5-7% of the world’s population carrying traits for thalassemia. However, the prevalence varies across regions. In India, thalassemia is a significant health concern, with an estimated 3-4% of the population being carriers of the thalassemia gene.
Thalassemia major, the most severe form, affects approximately 1 in 100,000 births worldwide, but the incidence is higher in populations where thalassemia carriers are more prevalent, such as in certain regions of India. β-Thalassemia is widespread in India, with carriers averaging a frequency of 3-4%. Certain communities, including Sindhis, Punjabis, Gujaratis, Bengalis, Mahars, Kolis, Saraswats, Lohanas, and Gaurs, exhibit a higher prevalence, as observed with frequencies of 6-7%.
These figures underscore the importance of awareness, carrier screening, and genetic counselling for thalassemia in and the impact of thalassemia on affected individuals and families.
What are the causes of Thalassemia?
Thalassemia is primarily caused by inherited genetic mutations (changes in the genes) that affect the production of haemoglobin, the essential protein in red blood cells. These mutations can be passed down from parents to their children. Simply put, think of genes as the body’s instruction manual for making haemoglobin. When there’s a change, or mutation, in these instructions, the body may struggle to produce the right amount of protein (alpha and beta globin chains), leading to an imbalance. This imbalance disrupts the normal process of creating healthy red blood cells, resulting in thalassemia.
What are the Symptoms of Thalassemia ?
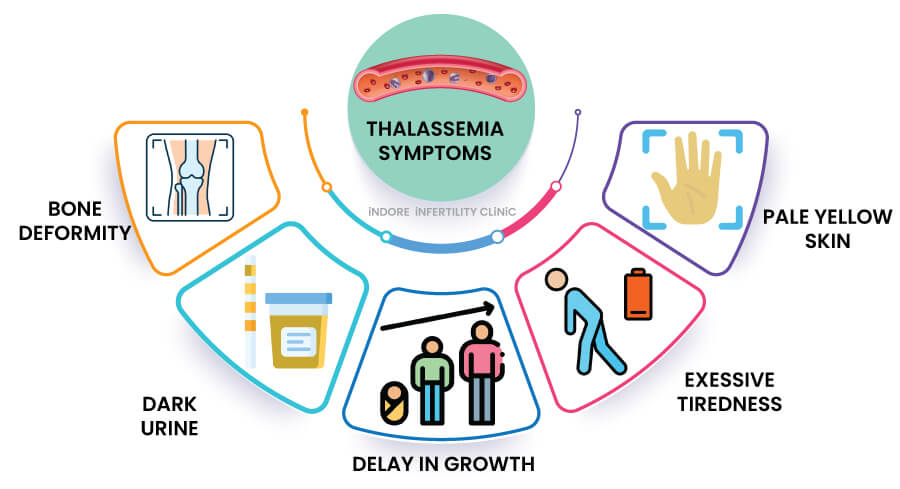
Thalassemia symptoms arise from a shortage of healthy red blood cells and decreased oxygen delivery throughout the body. Common symptoms include persistent fatigue and weakness. In more severe cases, individuals may have an enlarged spleen and liver, jaundice (yellowing of the skin and eyes), and bone deformities. Thalassemia can also increase the susceptibility to infections. It’s crucial for individuals experiencing these symptoms, especially those with a family history of thalassemia, to seek medical attention for a proper diagnosis and appropriate management.
Common symptoms of thalassemia are:
- Persistent Fatigue: Thalassemia causes chronic fatigue and weakness due to a shortage of healthy red blood cells, impacting the body’s oxygen supply.
- Enlarged Spleen and Liver: Thalassemia can lead to the enlargement of the spleen and liver, affecting their normal functions.
- Jaundice: In more severe cases, thalassemia may cause jaundice, characterized by yellowing of the skin and eyes.
- Bone Deformities: Severe forms of thalassemia can contribute to bone problems and deformities.
- Increased Infection Risk: Thalassemia may weaken the immune system, making individuals more vulnerable to infections.
It is important to recognize thalassemia-related signs, especially for individuals with a family history of the condition. Seeking medical attention for a proper diagnosis and appropriate management is crucial in addressing thalassemia-related health concerns. Regular check-ups and genetic testing in can aid in early detection and intervention specially if planning for pregnancy.
What are the types of Thalassemia and their genetic basis?
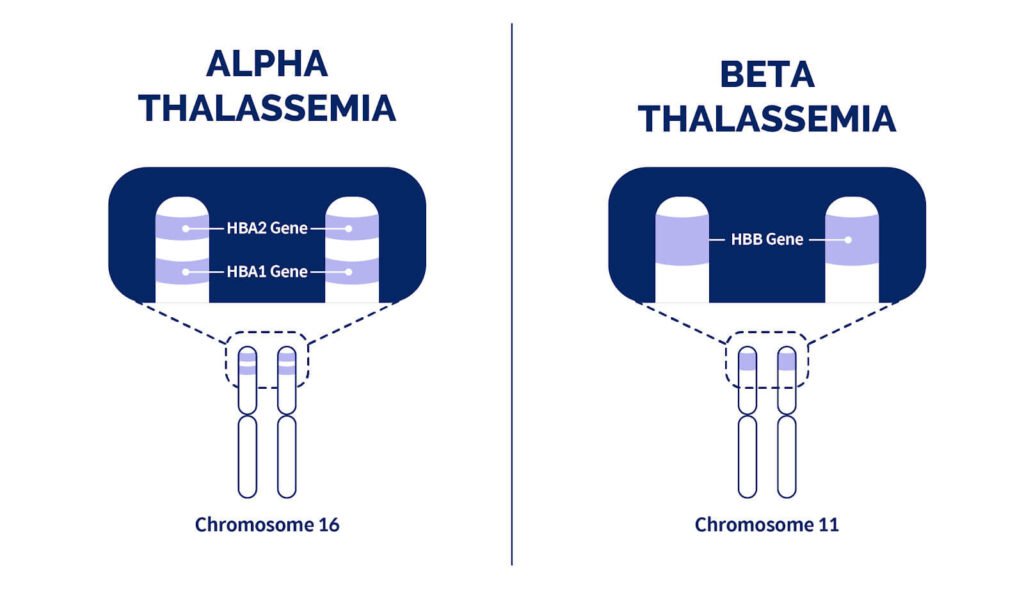
Thalassemia comes in two main types: alpha thalassemia and beta thalassemia, each with different genetic roots.
Alpha Thalassemia: This type results from a mutation in the genes that provide instructions for making alpha-globin chains. Depending on the number of affected genes, it’s classified as silent carrier, trait, or major (explained below).
Beta Thalassemia: This type stems from mutations in the genes guiding beta-globin chain production. It has three main forms: thalassemia major (severe), thalassemia intermedia (moderate), and thalassemia minor (mild).
Thalassemia Carrier is a person who has the abnormal gene which causes the disease, but they do not show the symptoms of the condition. They can pass on the condition to their children.
The condition arises from mutations which are inherited in the genes responsible for making haemoglobin, leading to an imbalance in the production of its components—alpha and beta globin chains. Depending on the specific gene mutations, thalassemia can result in a shortage of one or both types of these chains, disrupting the normal formation of red blood cells.
Which test is done for thalassemia or How is Thalassemia detected ?
The primary test for diagnosing thalassemia is called haemoglobin electrophoresis (Hb electrophoresis). This test identifies and quantifies the different types of haemoglobin in the blood, helping to determine if there’s an imbalance in the alpha and beta globin chains. Based on the results, doctors can classify the type and severity of thalassemia.
Additionally, genetic testing is often performed to identify specific mutations in the genes associated with thalassemia. This helps in confirming the diagnosis, understanding the genetic basis, and providing valuable information for family planning and genetic counselling for thalassemia.
At Indore Infertility Clinic, Indore we provide counselling, prenatal screening and also solutions to couples who have thalassemia or are at risk of having an affected baby. These tests, along with a thorough medical history and physical examination, play a crucial role in diagnosing and managing thalassemia.
What is the cost of thalassemia test ?
The cost of thalassemia testing in India can vary depending on the type of test and the diagnostic facility or laboratory where it is conducted. Generally, the cost for a basic haemoglobin electrophoresis test, which is the primary test for diagnosing thalassemia, can range from INR 500 to INR 2000 or more, depending on the location and the healthcare provider. The cost of Hb electrophoresis test for thalassemia at Indore is roughly INR 1000.
The genetic test for thalassemia mutation, which provides information about the exact haemoglobin type in a person can cost between INR 7000-10,000 depending on the city of residence and the laboratory.

How do I know if my baby has thalassemia?
During pregnancy, identifying the risk of thalassemia in your baby involves a combination of family history assessment, prenatal screening, and genetic testing. Here are the key steps which we follow at Indore Infertility Clinic to ensure a safe pregnancy for you:
- Family History Assessment: If you or your partner have a family history of thalassemia or belong to a population with a higher prevalence of thalassemia carriers, inform your doctor during preconception (before getting pregnant) or early pregnancy visits.
- Partner Screening: If one parent is identified as a carrier, it’s advisable to screen the other partner. The combination of specific carriers influences the risk of thalassemia in the baby.
- Prenatal Screening of the mother: Your doctor may recommend early pregnancy screening, including a complete blood count (CBC) and haemoglobin electrophoresis. Abnormal results may prompt further investigation.
- Non-Invasive Prenatal Testing (NIPT): This blood test analyses cell-free DNA from the fetus present in the mother’s blood. This test can indicate if your baby is at higher risk of thalassemia, but it is not confirmatory.
- Genetic counselling for thalassemia in: If screening indicates a potential risk, then genetic counselling for thalassemia is offered. A genetic counsellor can provide detailed information about the risk of thalassemia based on family history and screening results.
- Ultrasound: While not a direct genetic test for thalassemia, ultrasound can help identify certain physical abnormalities associated with severe forms of the disorder.
- Chorionic Villus Sampling (CVS): CVS is typically performed between 10 and 13 weeks of pregnancy. It involves taking a small sample of placental tissue for genetic testing in. This test can identify specific genetic conditions, including thalassemia.
- Amniocentesis: Usually performed between 15 and 20 weeks of pregnancy.
Involves collecting a sample of the amniotic fluid surrounding the fetus.
Genetic testing in on the cells in the fluid can reveal the presence of thalassemia.
By taking these steps, you and your doctor can assess the risk early in the pregnancy and implement appropriate measures for managing and planning the care of your baby, ensuring the best possible outcome.
Why your family history matters in Thalassemia risk?
Your family history is a vital piece of the puzzle when it comes to understanding the risk of thalassemia. Thalassemia is a genetic disorder, meaning it’s passed down through parents. If one or both parents carry the thalassemia gene, there’s a risk of passing it on to their children. Your family history provides valuable clues about the presence of thalassemia in your lineage. If there’s a history of thalassemia carriers or individuals with thalassemia in your family, it raises the likelihood of the gene being present in you and eventually your baby.
Here’s why your family history matters:
- Inherited Nature: Thalassemia is inherited, and a family history of the condition increases the likelihood of carrying the gene.
- Carrier Identification: Knowledge of thalassemia in your family helps identify potential carriers. Carriers may not show symptoms but can pass the gene to their children.
- Risk Assessment: Understanding the family history allows your doctor to assess the risk early in pregnancy, enabling timely interventions and appropriate care.
- Genetic counselling for thalassemia: Genetic counselling for thalassemia becomes more precise with family history. It helps you make informed decisions about testing, family planning, and potential implications for your children.
By sharing your family history with your doctor and seeking genetic counselling for thalassemia at Indore Infertility Clinic, you empower yourself to navigate the complexities of thalassemia, ensuring the best possible outcomes for your family.
Can I marry a thalassemia patient ?
The decision to marry a person with thalassemia is a personal one and involves careful consideration of various factors.
Here are key points to consider before proceeding:
- Understanding Thalassemia Types: Thalassemia comes in different types and severities. Understanding the specific type and its impact on the individual is crucial.
- Genetic Compatibility: If you and your partner both carry the thalassemia gene, there’s a risk of having a child with thalassemia. Genetic testing and counselling can provide insights into this risk. However, if you opt for IVF with PGT ( preimplantation genetic testing), you can transfer only those embryos that do not carry both defective gene and plan a pregnancy)
- Genetic counselling for thalassemia: Seeking genetic counselling for thalassemia as a couple can provide detailed information about the risk of having a child with thalassemia and assist in making informed decisions.
- Medical Advances: Advances in medical treatments and technologies, such as pre-implantation genetic diagnosis (PGD) and prenatal testing, offer options for managing the risk of thalassemia in offspring.
- Quality of Life: Consider the impact of thalassemia on your partner’s quality of life and the potential challenges you may face as a couple and as parents.
- Emotional Support: A supportive and understanding relationship is essential. Open communication about expectations, concerns, and plans for family-building is crucial.
Ultimately, the decision to marry a person with thalassemia involves weighing the emotional, medical, and practical aspects of the relationship.
Can Thalassemia patients conceive naturally?
Yes, individuals with thalassemia can conceive naturally. However, there are important considerations and potential challenges to be aware of:
- Fertility Issues: Thalassemia, especially in its more severe forms, may be associated with hormonal imbalances that can impact fertility. It’s essential for individuals with thalassemia to discuss fertility concerns with their gynaecologist or infertility specialist.
- Iron Overload: Thalassemia patients who have undergone multiple blood transfusions may experience iron overload, which can affect various organs, including the reproductive organs. Managing iron levels is crucial for overall health and fertility.
- Medication and Treatments: Some medications used to manage thalassemia, such as chelation therapy to reduce iron overload, may need to be adjusted during pregnancy. It’s important for individuals to work closely with their healthcare team to make dose adjustments or if needed switching to safer drugs to ensure a safe and healthy pregnancy.
- Genetic counselling for thalassemia: Thalassemia is an inherited genetic condition. Couples planning to have children should undergo genetic counselling for thalassemia to understand the risk of passing thalassemia to their offspring and to explore available options of testing.
In summary, while natural conception is possible for individuals with thalassemia, it’s important to approach pregnancy with careful planning, close medical supervision, and, if necessary, with the guidance of fertility specialists and genetic counsellors.
How does Thalassemia affect fertility and ability to have a baby ?
Thalassemia can impact fertility in several ways, although the degree of effect varies among individuals. Here are key factors to consider:
- Hormonal Imbalances: Thalassemia, particularly in its more severe forms, can lead to hormonal imbalances. Hormones play a crucial role in regulating the menstrual cycle and ovulation in women, and disruptions in this balance may affect fertility.
- Iron Overload: Regular blood transfusions, a common treatment for thalassemia, can lead to iron overload in the body. Excess iron can impact the endocrine system, potentially affecting fertility by disrupting normal hormonal function.
- Delayed Puberty: Thalassemia may cause delayed puberty due to hormonal imbalances, which can, in turn, affect the timing of the menstrual cycle and ovulation in women.
- Treatment-Related Factors: Medications used to manage thalassemia, such as chelation therapy to reduce iron overload, may have implications for fertility. It’s essential to consult with your doctor to understand the effects of specific treatments.
- Psychological Factors: Living with a chronic condition like thalassemia can lead to stress and psychological factors that may indirectly impact fertility.
Despite these potential challenges, many individuals with thalassemia can have successful pregnancies with appropriate medical guidance and support. It’s crucial for those with thalassemia who are considering pregnancy to work closely with doctors, including fertility specialists, if necessary, to address specific concerns and optimize the chances of a healthy conception and pregnancy.
What are the main causes of infertility in women and men with thalassemia?
Infertility in individuals with thalassemia can result from various factors, impacting both women and men. Here are the main causes:
In Women:
- Hormonal Imbalances due to Iron overload and endocrine dysfunction: Thalassemia, especially in its more severe forms, can disrupt hormonal balance, affecting the regularity of menstrual cycles and ovulation.
- Delayed Puberty: Thalassemia may lead to delayed puberty, influencing the timing of the menstrual cycle and ovulation.
- Ovarian Damage: Iron deposition in the ovaries can cause damage to ovarian tissue, potentially affecting the quality of eggs.
In Men:
- Hormonal Imbalances due to Iron overload and endocrine dysfunction: Thalassemia can disrupt the hormonal balance in men, affecting sperm production.
- Testicular Damage: Iron deposition in the testes can lead to damage, potentially impacting sperm quality and quantity.
- Erectile Dysfunction: Thalassemia-related complications or psychological factors may contribute to erectile dysfunction, affecting fertility.
Understanding these potential causes is crucial for individuals with thalassemia facing fertility challenges. Consultation with fertility specialists, can help address specific concerns, explore treatment options, and provide guidance for optimizing the chance of a healthy pregnancy.
How does Thalassemia affect pregnancy?
Thalassemia can affect pregnancy in various ways.
Here are key aspects to be aware of:
- Risk of Genetic Transmission: Thalassemia is an inherited genetic condition. If both parents are carriers, there’s a risk of passing thalassemia to the child. Genetic counselling for thalassemia is provided at Indore Infertility Clinic and further testing can help assess this risk.
- Iron Overload: Regular blood transfusions, a common treatment for thalassemia, can lead to iron overload in the body. Managing iron levels during pregnancy is crucial to prevent complications.
- Increased Monitoring: Pregnancies in individuals with thalassemia often require increased medical monitoring. Regular check-ups, blood tests, and ultrasound examinations are essential to assess both maternal and fetal well-being.
- Complications for Thalassemia Major: Women with thalassemia major (severe form) may face additional challenges during pregnancy due to the underlying health condition. Close collaboration between obstetricians and haematologists is essential to ensure healthy pregnancy.
- Blood Transfusions during Pregnancy: In some cases, individuals with thalassemia may require blood transfusions during pregnancy to maintain optimal haemoglobin levels.
Overall, with proper medical care, monitoring, and support, many individuals with thalassemia can have successful pregnancies. It’s essential to work closely with a healthcare team, including fertility specialists, haematologists and obstetricians, to navigate the unique complications associated with pregnancy in individuals with thalassemia.
Can Thalassemia be passed down to children ?
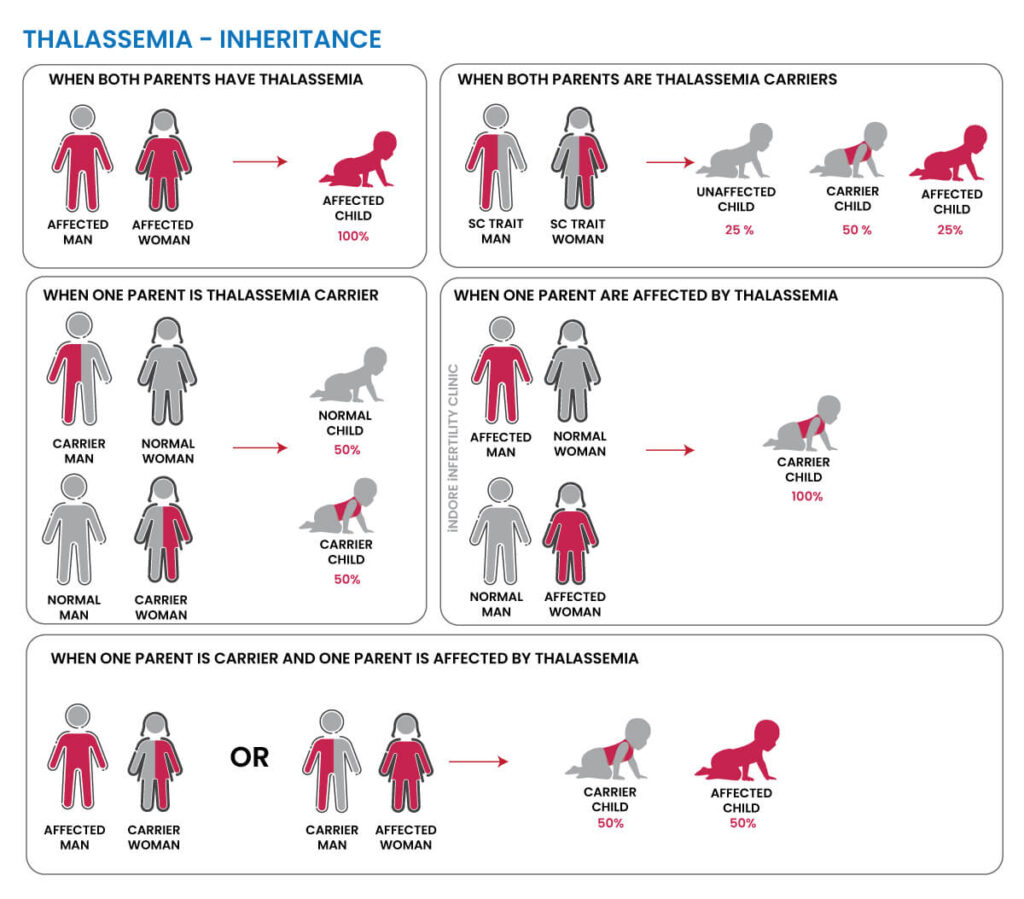
Yes, thalassemia is an inherited genetic condition, and it can be passed down from parents to their children. Thalassemia is caused by mutations in the genes responsible for producing haemoglobin—the protein in red blood cells that carries oxygen. There are two main types of thalassemia: alpha thalassemia and beta thalassemia.
How is Thalassemia Inherited:
- If both parents are carriers (have one mutated gene), there is a 25% chance with each pregnancy that their child will inherit thalassemia (have two mutated genes) and be affected by the condition.
- If one parent is a carrier and the other is not, there is a 50% chance that each child will be a carrier, but they will not have thalassemia.
- If both parents are carriers of different types of thalassemia, their children may inherit a combination of the mutations, leading to various forms and severities of thalassemia.
- If both parents are affected by similar type of thalassemia, all children will inherit the disease and will be affected by thalassemia.
Remember – Carrier is a person who has the abnormal gene which causes the disease, but they do not show the symptoms of the condition. They can pass on the condition to their children.
What types of Preimplantation genetic diagnosis available for Thalassemia?
Preimplantation genetic diagnosis for thalassemia (PGT) is a method used during in vitro fertilization (IVF) to examine embryos for genetic disorders before they are implanted into the uterus. For thalassemia, specifically, the types of that can be employed are:
PGT-M (Preimplantation genetic testing for Monogenic Disorders): PGT-M is used to detect specific genetic mutations, such as those causing thalassemia. It allows for the identification of embryos that are free from thalassemia mutations, reducing the risk of transmitting the disorder to the offspring.
PGT-SR (Preimplantation genetic testing for Structural Rearrangements): PGT-SR is used when there are structural rearrangements in the chromosomes that may be linked to thalassemia. It helps identify embryos with normal chromosomal structures.
Process:
- During IVF, embryos are created in a laboratory.
- A few cells are removed from each embryo.
- These cells are then tested for the specific thalassemia mutation or chromosomal rearrangement.
- Only embryos without the identified genetic issues are selected for implantation.
Benefits:
- PGT offers the opportunity to select embryos that are not affected by thalassemia, reducing the risk of having a child with the condition.
- It allows for family planning with a greater degree of certainty and control.
Individuals or couples considering PGT for Thalassemia in Indore for should consult with our fertility specialist at Indore Infertility Clinic and also consult genetic counsellor to discuss the specific details of their situation and the available options.
Preventing Thalassemia through IVF and Genetic Screening
Preventing thalassemia through IVF (in vitro fertilization) and genetic screening involves a process known as Preimplantation genetic diagnosis thalassemia for Monogenic Disorders (PGT-M).
Here’s an overview of the steps involved, that we follow at Indore Infertility Clinic:
Genetic counselling for thalassemia: Couples with a family history of thalassemia or those identified as carriers or affected by thalassemia should seek genetic counselling for thalassemia. This involves a discussion with a genetic counsellor who can explain the inheritance pattern, assess the risk, and discuss available options.
- Carrier Screening: Both partners undergo carrier screening to identify if they carry a mutation for thalassemia. If both are carriers, there is a risk of having a child with thalassemia.
- In Vitro Fertilization (IVF): IVF is a fertility treatment where eggs and sperm are combined outside the body (in a laboratory) to create embryos.
- Embryo Creation: Eggs are retrieved from the woman and fertilized with sperm in a laboratory, creating embryos.
- embryo Biopsy: A few cells are removed from each embryo.
- Genetic testing (PGT-M): The removed cells are tested for thalassemia mutations using PGT-M. This identifies embryos that are free from thalassemia mutations.
- Selection of Healthy Embryos: Only embryos without thalassemia mutations are selected for implantation.
- Implantation: Selected embryos are implanted into the woman’s uterus.
- Pregnancy: If successful, the baby will be free from the risk of thalassemia, as only embryos without the mutation are implanted.
Benefits: This process allows couples at risk of thalassemia to have children who are not affected by the disorder. It provides a way to prevent the transmission of thalassemia to future generations.




