
Is laparoscopy advised to all infertility patients ?
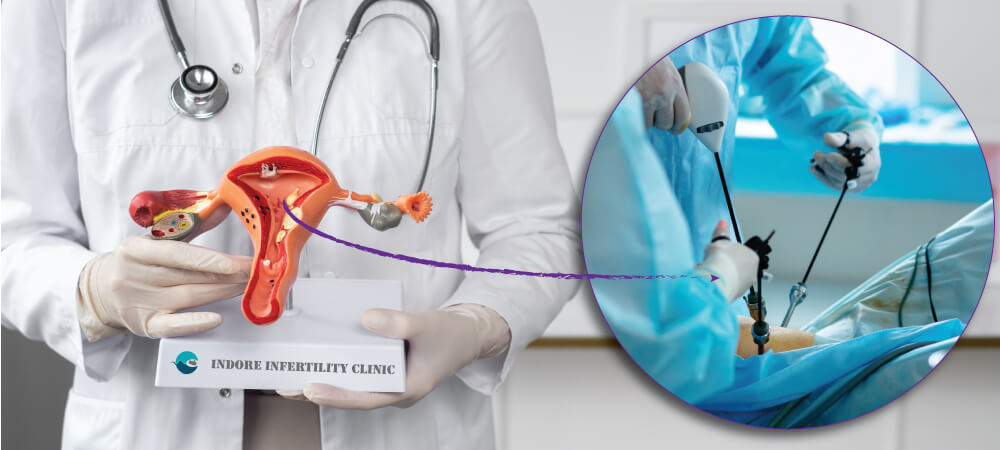
Laparoscopy is advised usually in order to find the cause of infertility – whether it is because of tubal cause or if there are any structural anomalies to the fallopian tube, ovaries or uterus. Laparoscopy is advised, if a patient is not able to conceive in spite of all other reports being normal. The procedure is known as Diagnostic Laparoscopy – where the intention is to diagnose the cause of infertility.What are the benefits of laparoscopy over traditional tests like USG and HSG to assess the female reproductive health?
During laparoscopy, a laparoscope is able to capture HD image and video of the entire pelvic cavity in real time, it makes diagnosis of infertility very easy and accurate. It is like seeing the inside view of the patient’s organs. Tests like USG and HSG do have ability to diagnose the cause of infertility to some extent, but it is like seeing a shadow of an organ, while laparoscopy allows Infertility specialist to view the actual organs in real time.Does it make sense to undergo laparoscopy without wasting time for patients of Unexplained Infertility?
Cases of Unexplained Infertility are very difficult to diagnose by routine tests since most of the reports like Semen Analysis, Follicular Monitoring and baseline Ultrasound comes out normal. This makes it very difficult for patients to accept their infertility. Baseline ultrasound is good for assessment of endometrium and general structure of Uterus. It is also useful for monitoring ovulatory function. HSG on the other hand is useful for testing patency of tubes (whether fallopian tube is open or blocked). However, HSG test is not useful for diagnosis of tubal adhesions or infection in fallopian tube. Laparoscopy, allows Infertility specialist to not only test the patency of tube, but also allows them to rule out tubal adhesions. Tubal adhesions can disrupt the path and connection between ovaries and uterus, which may lead to the egg not reaching the fallopian tube after being released and hence no pregnancy is achieved leading to infertility. Tubal cysts and tubercles are structures that are at times present in the fallopian tube but not visible on an Ultrasound. Tubercles are small structures that are visible during laparoscopy and are sign of Tuberculosis. Tubal TB if untreated can lead to infertility. Laparoscopy also allows an IVF specialist to assess grade of endometriosis, a chronic condition that affects reproductive health of a female. Assessment of grade of endometriosis helps an IVF specialist to plan out the fertility drug based on the extent of endometriosis to yield better result to the treatment cycle. During laparoscopy ovarian cysts can also be aspirated. Hence at times especially when the female age is nearing 30 or there is a reason to suspect infection or adhesions, it is advisable to undergo diagnostic laparoscopy right away.Is laparoscopy painful?
Laparoscopy is performed under general anesthesia and usually takes about 15 to 20 minutes. It is minimally invasive procedure leaving behind a tiny incision that can be sutured using two to three stiches. Post laparoscopy, patients are prescribed pain killers for 2 to 3 days. Patients usually feel a little discomfort after laparoscopy, but generally do not feel severe pain.
What precautions should I take after undergoing laparoscopy?
Laparoscopy being a minimally invasive procedure does not require for a patient to take too many precautions. However, it is always advisable to not undertake severe form of exercise etc. immediately after the procedure. Patients can continue their routine work after the procedure.
How many days leave should I plan for undergoing laparoscopy?
Patients are typically discharged on the same day after the procedure. Laparoscopy is an outpatient procedure needing no hospitalization. However, once discharged, make sure you take your prescribed painkillers and antibiotics for 2 to 3 days or as prescribed by your doctor.
Do I need bed rest after laparoscopy?
Typically not. Patients do not need any bedrest after laparoscopy. Patients typically feel minor discomfort for two to three days which settles on their own. Make sure to eat healthy food and sleep well for 3 to 4 days after the procedure.
What is the cost of laparoscopy?
The cost of laparoscopy is around INR 30 to 35 K.
What is the difference between laparoscopy and hysteroscopy?
Laparoscopy involves inserting a laparoscope by making a small incision under the belly button, this helps a specialist to visualize the entire pelvic cavity including reproductive organs like the ovaries, fallopian tube and outside of the uterus.
Hysteroscopy involves inserting a hysteroscope through the vaginal cavity which helps the specialist to visualize the internal uterine structure and the opening of the fallopian tubes from the uterus. Hysteroscope is an instrument like a laparoscope which also has an HD Camera attached to it.
What is hystero-laparo?
Hystero-Laparo is short form of Hysteroscopy combined with Laparoscopy. During this process both laparoscope as well as hysteroscope is inserted to assess the reproductive organs. In cases of Unexplained Infertility it makes sense to combine both laparoscopy and hysteroscopy for complete assessment of the Uterus, endometrium, opening of the fallopian tube, the ovaries and the fallopian tubes.

Can I plan pregnancy immediately after laparoscopy?
Yes, you can plan your pregnancy during the next cycle.
How long should one wait after laparoscopy before planning IVF cycle?
You can plan your IVF cycle from the very next menstrual cycle after laparoscopy.
Does IVF Success Rate improve after Laparoscopy ?
There is no evidence that suggests the same. However if during a diagnostic laparoscopy some uterine or structural anomaly has been corrected it may result in better implantation rates and hence better success rate of IVF.
Does egg quality improve after laparoscopy?
No data suggests that it does. Laparoscopy or hysteroscopy does not impact the quality of eggs in the ovaries.
Are there any known complications or risks after laparoscopy?
Apart from the regular risks associated with General Anesthesia, laparoscopy or hysteroscopy does involve a minimal risk of infection or bleeding.
Will I be on any long term medication after laparoscopy?
You shall be prescribed painkillers and short course of antibiotics for 3 to 5 days after laparoscopy.