
Why does IVF Fail?
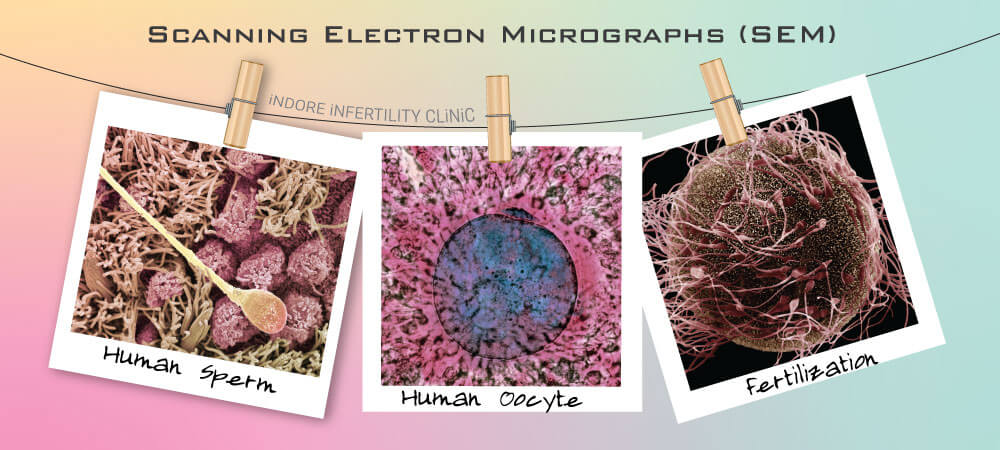
Mathematically speaking, a good quality oocyte (egg) when fertilised with a good sperm should lead to a good embryo.
When such a good quality embryo is transferred to a good uterus with a good endometrial lining or thickness, it should result in a positive beta hcg and a subsequent healthy pregnancy. When everything falls into place, such a pregnancy will result into birth of a healthy child.
Sounds simple, right!
But this in itself has about hundreds of interdependent and independent factors.
The success of an IVF cycle depends on close correlation of these factors with each other. One factor out of control may impact the result of the entire cycle and lead to a Failed IVF cycle.
So, what are the factors that impact the success of an IVF Cycle?
What can cause IVF to Fail ?
what are the reasons for failed IVF ?
Listing some of the factors here:
- Quality of oocyte or egg – Quality of not only the genetic material, but also the cytoplasmic content of the oocyte.
- Quality of sperm – Mostly the quality of packaging of the DNA within the sperm’s head.
- The protocol and drug used to stimulate the ovaries to produce mature oocytes. There are many protocols that can be used to achieve the same end result, however the choice of the Stimulation Protocol, the choice of the exact drug used for stimulation, the number of days a patient needs to be stimulated – All these factors impact the number and maturity of oocytes retrieved at the end of egg retrieval. This is one of the most important aspects of the IVF cycle and needs years of experience by a well seasoned Infertility Specialist to master and individualize.
- The drug(s) used to trigger the ovaries prior to ovulation and the timing of the egg retrieval with respect to injection of these drugs.
- Factors within the IVF Lab
- Choice of method used for fertilization. This is a crucial step that depends on the assessment of sperm function and ovarian reserve.
- Timing of insemination during IVF or ICSI with respect to administration of trigger shot.
- Method used for sperm preparation prior to IVF or ICSI – swim up or density gradient.
- Timing of insemination / ICSI with respect to Trigger and OPU
- The skill level of the Embryologist performing ICSI and IVF insemination and gamete handling.
- Embryo Culture Strategy used to culture the fertilized embryos.
- The embryo culture medium used to culture embryos.
- The embryo culture environment within the IVF lab that includes the type of incubator (low oxygen humidified incubators are preferred), the embryo culture media, air quality, light source etc.
- The embryo assessment, segregation and handling strategies.
- Embryo Freezing and Warming technique along with the freezing and warming media.
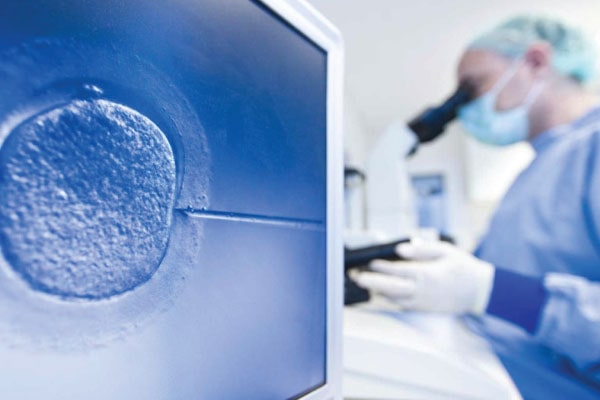

- Embryo Transfer Technique in itself.
- Transferring Embryo by close assessment of implantation window and endometrial receptivity prior to Embryo transfer.
- Choice of luteal phase support provided after the Embryo Transfer
- Factors that cannot be controlled:
• Genetic abnormalities arising within the embryo after fertilization.
• Poor cross-talk between Embryo and endometrium leading to failed implantation.
What can be done differently in the next IVF Cycle in case of previous failed IVF Cycle?
TRY AND IMPACT THE QUALITY OF GAMETES (SPERM AND OOCYTE QUALITY)
It is a known fact that quality of oocytes and sperms are dependent on age, diet and exercise. You cannot reverse your age, however you can plan to eat balanced diet and exercise. Try and achieve a healthy BMI. Antioxidants to reduce Reactive Oxidative stress (ROS) on sperms and eggs can also be tried.
TRY A MORE PERSONALIZED IVF STIMULATION PROTOCOL
Stimulation protocol for poor ovarian reserve is different from the stimulation protocol used in patients who have Polycystic ovaries or PCOS. Drugs used during the stimulation protocol directly impact folliculogenesis (process of formation of ovarian follicle) and oogenesis (process of maturation of oocytes).
The entire process of ovarian stimulation needs to occur in close monitoring with ultrasound finding so that appropriate drug can be given at the right time. It hence makes sense to have the same person do the ultrasound as well as decide the timing and dosage of stimulation drug.

CAREFULLY COORDINATED TIME OF TRIGGER AND OVUM PICKUP (OPU OR EGG RETREIVAL)
A successful ovarian stimulation ends with proper maturity of ovarian follicles which are then triggered by either a single drug or a combination of drugs (Dual Trigger or Single Trigger) to initiate final maturity of oocytes (eggs). The procedure to collect eggs (Oocyte Retrieval or Ovum PickUp) is timed 34 to 36 hrs after the trigger shot. The timing of OPU with respect to the trigger is of utmost importance and leads to retrieval of mature oocytes. Every minute matters.
TRY A DIFFERENT EMBRYO CULTURE STRATEGY
Cases of previous IVF Failure need to be meticulously planned by inspecting all parameters of previous IVF Cycle. In case of previous Embryo transfer on Day 3, extended culture on Day 5 ( Blastocyst Culture) should be planned. Freeze All IVF Protocol is used in many cases for patients with poor ovarian reserve or cases of Ovarian Hyper Stimulation (OHSS).
IVF LAB PRACTICES
- Try using of capacitated sperms.
- Try a different sperm selection method like microfluidic channel based on sperm function test result.
- Try different culture protocol based on knowledge of what was used previously.
- Choose extended culture of embryos till Blastocyst Stage (Day 5 ) and Single Blastocyst Embryo Transfer.
- Choose a lab that shows transparency in services by sharing status of the entire process from egg collection to embryo transfer with or without images.
- More synchronized Embryo Transfer with respect to implantation window.
CROSS CHECK LUTEAL PHASE SUPPORT AND ENDOMETRIAL PREPARATION
- Try a different regimen for luteal phase support.
For problem with endometrial lining try PRP Therapy with or without endometrial scratching.
For Recurrent Implantation Failures, low molecular weight heparin and low dose aspirin can be added after embryo transfer. - If Hysteroscopy has not been done, it should be done prior to embryo transfer to rule out endometrial polyps which can be missed on ultrasound.
- Bed rest after Embryo Transfer reduces chances of pregnancy, so adequate ambulation (movement and activity) is recommended.
- Hydrosalpinx (dilated and fluid filled fallopian tubes) can also lead to IVF Failure. Tubal Clipping or delinking is recommended in such cases.
- Endometrial Biopsy for TBPCR should be done to rule out endometrial infection which is asymptomatic in many cases.




